만성비염 환자에서 항원감작 여부에 따른 환자 특성 파악
Patients’ Characteristics according to Allergic Sensitization in Chronic Rhinitis
Article information
Trans Abstract
Background and Objectives
Chronic rhinitis is divided into allergic rhinitis (AR) and nonallergic rhinitis (NAR), both of which have similar symptoms but differ in treatment approaches. For the diagnosis of AR, allergen-specific immunoglobulin E (IgE) tests along with characteristic symptoms are required. However, these tests are costly and not always practicable. The purpose of this study was to investigate how symptoms respond differently to different allergen sensitization or sensitized allergen.
Subjects and Method
We retrospectively reviewed 1661 patients who underwent multiple allergen simultaneous test (MAST) for chronic rhinitis symptoms. The total nasal symptom (TNS) scores of these patients from 2006 to 2014 were assessed for rhinorrhea, nasal obstruction, itching, and sneezing. Patients were classified as AR and NAR according to the results of MAST and their association with symptoms.
Results
There were 1021 patients designated to the AR group and 640 patients to the NAR. The AR group had lower age, higher TNS, and higher serum IgE levels than the NAR group. In addition, sneezing and itching were more common in the AR group. Furthermore, sneezing was a positive predictor for seasonal allergen sensitization. On the other hand, itching was a positive predictor for perennial allergen sensitization.
Conclusion
AR and NAR patients showed different demographic characteristics and symptoms. These results may be helpful in classifying and treating patients with chronic rhinitis, especially when the allergen specific IgE test cannot be performed.
Introduction
Chronic rhinitis is a common disorder which can affect patient’s quality of life and social activities. It comprises heterogeneous diseases and is classified as allergic rhinitis (AR) or non-allergic rhinitis (NAR). Although, both AR and NAR showed similar nasal symptoms [1], the treatment strategies for the patients may differ. Physicians may recommend allergen avoidance or immune therapy to AR patients according to guidelines [2]. In addition, according to sensitized allergen, the ways of allergen avoidance are different.
The diagnosis of AR is made on the basis of characteristic symptoms and the test for allergen-specific immunoglobulin E (IgE) such as multiple allergen simultaneous test (MAST) or skin prick test [3]. However, these tests are time and money consuming for both the patient and the doctor. In addition, it is not always possible to evaluate the allergen specific IgE, especially for the primary physician.
In this study, we attempted to identify the clinical clue for differentiating the patients with chronic rhinitis according to allergic sensitization or type of sensitized allergen. Patients with characteristic rhinitis symptoms were enrolled and their symptom, age, gender and urbanization level of their residence were analyzed.
Subjects and Method
Retrospective chart reviews were performed for patients who visited the ENT clinic with chronic rhinitis symptoms from July 2006 to June 2014. Presence and prevalence of each of the 4 nasal symptoms (rhinorrhea, nasal obstruction, itching and sneezing) were investigated. The scores were rated as 1 or 0 according to the presence or absence of patient’s symptom. Total nasal symptom (TNS) score of patients was defined as the number of symptoms complained of by patients (1-4). Patients without any nasal symptom were excluded from the study. Ratio of specific symptom among all symptoms was defined as the relative ratio. Relative ratios for each nasal symptom score among the TNS score were analyzed.
Serum total IgE was assessed. Testing for allergen-specific IgEs was done with MAST. Patients with a positive test result for inhalant allergens were classified into the AR group and patients with a negative test result for inhalant allergens were classified into the NAR group. Reactions equal or more than class 2 (≥0.7 IU/mL) were considered positive. According to the characteristics of allergens, allergens were classified and analyzed as seasonal allergens and perennial allergens. Seasonal allergens included pollen, trees, grass pollen and weeds. Perennial allergens included dust mites, cockroaches, animal dander, and fungi or mold [4]. In this study, an area with a population density of more than 1000 people per square kilometer was defined as an urban region. The Institutional Review Board approved this study protocol (#CNUH-2015-260).
Statistical analysis
The chi-square test was used to compare categorical variables between the AR group and NAR group. The independent sample t-test was used to compare continuous variables such as age and serum total IgE. To identify the factor associated to according to the type of sensitized allergen, multivariate regression tests were performed. All statistical analyses were performed using IBM SPSS Statistics for Windows ver 20.0 (IBM Corp., Armonk, NY, USA). Two-sided p values <0.05 were considered statistically significant.
Results
A total of 1661 patients were enrolled in this study. The mean age of the study population was 33.6±18.8 years. One thousand and twenty-one (61.5%) patients were sensitized to a specific allergen and 640 (38.5%) patients showed a negative MAST result. D. pteronyssinus showed the highest sensitization rate among the 39 allergens. Allergen sensitization rates decreased with age (Supplementary Fig. 1). The AR group showed a significantly lower age, male dominance, more nasal symptoms, and higher serum total IgE level (Table 1). The prevalence of AR decreased with age and the prevalence of NAR increased with age (Supplementary Fig. 1).
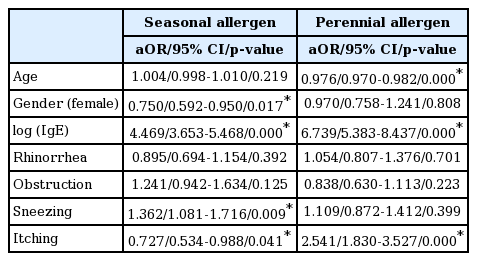
We analyzed data according to the type of allergen. Allergens were classified into seasonal allergens and perennial allergens. To identify factors for allergic sensitization according to the type of allergens, we performed a multiple regression test (Table 2). Sneezing was a positive predictor for seasonal allergen sensitization [SAR, p=0.009, adjusted odds ratio (aOR)=1.362, 95% confidence interval (CI): 1.081-1.716] and itching was a negative predictor for SAR (aOR=0.727, 95% CI: 0.534-0.988, p=0.041). For perennial allegen sensitization (PAR), itching was the only positive predictor (p=0.000, aOR=2.541, 95% CI: 1.830-3.527). Rhinorrhea and nasal obstruction were not predictive factors for AR, NAR, SAR and PAR. Seasonal allergies peaked at a person’s 40 s (Fig. 1). However, the number of sensitized perennial allergens decreased with age.

The number of sensitized allergens according to the age group. Although the number of sensitized perennial allergens decreased with age, the number of sensitized seasonal allergens peaked in a person’s 40s.
We analyzed the nasal symptom according to the age group. Prevalence of four nasal symptoms peaked in patients who were in their 10s and 20s and it decreased with age (Fig. 2). However, relative ratio for each symptom showed that itching decreased with age and rhinorrhea increased with age (Supplementary Fig. 2).

The prevalence of 4 nasal symptoms according to the age group. Itching decreased with age. Sneezing was increased in middle age groups.
969 (58.3%) patients were from urban regions and 692 (41.7%) patients were from rural regions. There was no difference in gender, total IgE, overall allergic sensitization rate, and TNS score between the two groups. However, the mean age, the number of sensitized seasonal allergens and prevalence of sneezing were significantly higher in the rural group (p=0.000, 0.045, 0.027, respectively). The prevalence of PAR showed no difference according to urbanization (Supplementary Table 1).
Discussion
Chronic rhinitis symptoms are among the most common problems presenting to physicians [5]. It is classified into AR and NAR. Although both AR and NAR show similar nasal symptoms [1], the treatment strategies for patients may differ. Physicians may recommend allergen avoidance or immune therapy to AR patients according to guidelines [2]. In addition, the ways of allergen avoidance differ according to the sensitized allergen. Therefore, this study classified AR into SAR and PAR according to the types of sensitized allergen, in spite of the fact that the current classification classifies the severity of AR into intermittent/persistent and mild/moderate to severe [6].
Not all patients with IgE-sensitization have AR. The diagnosis of AR is made on the basis of characteristic symptoms and the test for allergen-specific IgE such as MAST or skin prick test [3,7]. NAR is diagnosed by ruling out other causes of AR. We only enrolled patients with chronic rhinitis symptoms; rhinorrhea, nasal obstruction, sneezing and itching. Therefore, in this study, patients who were sensitized to inhalant allergens were classified into the AR group, whereas, Patients with a negative test result were classified into the NAR group.
We analyzed clinical characteristics and symptoms according to the type of sensitized allergen. Characteristics of the AR group were younger age, male dominance, higher total IgE level and higher TNS score. However, detailed analysis regarding the 4 nasal symptoms showed that sneezing and itching were specific symptoms of AR. There was no difference in rhinorrhea and nasal obstruction between the AR and NAR groups. A more interesting result was that SAR and PAR presented with different nasal symptoms.
We supposed that the characteristic of SAR was sneezing. First, sneezing was a statistically significant factor for predicting SAR in multiple regression test (Table 2). However, itching was a negative predictive factor for SAR. Second, the number of sensitized seasonal allergens according to the age group (Fig. 1) and prevalence of sneezing according to the age group (Fig. 2) showed a similar pattern. Thirdly, sneezing was the only symptom which showed a difference between rural and urban patients. In a rural area, there are numerous seasonal allergens. The number of sensitized seasonal allergens was significantly higher in rural areas.
There are debates regarding the prevalence of AR according to age. Some authors have reported that they did not find a significant increase in the prevalence of NAR with increased age [8]. However, our study showed a different result. Although SAR and PAR showed a different pattern, the overall rate of allergic sensitization in chronic rhinitis was found to decrease with age (Supplementary Fig. 1). The percentage of NAR was found to increase with age. Our result was in accordance with the finding of the study by Warm, et al. [9]. They also concluded that AR decreased with age. In addition, they stated that the decrease in AR according to age is an effect of normal aging and not primarily a birth cohort effect [9].
We analyzed the regional differences according to urbanization. Our study results showed that there was no regional difference in gender, level of total IgE, prevalence of allergic sensitization and TNSs (Supplementary data). In addition, there was no regional difference in the overall allergic sensitization rate. This result was in accordance with that in the study by Salo, et al. [10] who concluded that the overall prevalence of allergic sensitization does not vary across US. However, our study revealed that the number of sensitized seasonal allergens was larger in patients from rural regions (p=0.045). Higher chances of seasonal allergen exposure in rural areas may explain the larger number of sensitized allergens.
The limitation of this study is that MAST was used to test allergen sensitization. MAST has lower sensitivity and specificity than skin prick test. However, skin prick test requires multiple skin pricks and it causes discomfort to patients. The result of skin prick test can be influenced by medications. On the other side, MAST can be performed easily. It can be performed in younger patients and some physicians support the use of MAST as a diagnostic tool [11]. In addition, we performed the skin prick test in some patients with highly suspected AR with negative MAST result. However, there was no consistency in performing the skin prick test. So, we excluded the patient with skin prick test result.
The other limitation of this study is that the study did not subclassified the NAR group. There are many heterogeneous disease entities in NAR as Kaliner [12] mentnioned. However, due to the limitation in raw data of 1661 patients, we could not have subclassified patients according to disease entities.
Supplementary Materials
Acknowledgements
This research was supported by the Bio & Medical Technology Development Program of National Research Foundation of Korea (NRF) funded by the Korean government MSIP (NRF-2017M3A9E8023021).
This study was supported by a grant (CRI 15903-21) from Chonnam National University Hospital Biomedical Research Institute.