Post-Extubated Dysphagia in Intensive Care Unit Patients Based on Flexible Endoscopic Evaluation of Swallowing Examination and Its Affecting Factors
Article information
Abstract
Background and Objectives
Post-extubation dysphagia (PED) is a condition characterized by swallowing difficulty following the removal of breathing tube. Untreated dysphagia leads to increased morbidity and mortality; however, no study has been conducted on the proportion of PED at RSUPN Dr. Cipto Mangunkusumo (RSCM), using flexible endoscopic evaluation of swallowing (FEES), or on the factors that contribute to its occurrence.
Subjects and Method
Anamnesis and medical record review were conducted on post-extubation patients in the RSCM intensive care unit (ICU) meeting inclusion criteria. Research subjects underwent maximum phonation time (MPT) examination thrice. FEES examination was carried out twice, with 24 hours of post-extubation on all subjects and 72 hours of postextubation on those with PED on initial FEES examination.
Results
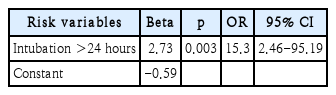
The study involved 33 subjects who met the inclusion criteria. The proportion of mild to severe PED determined by FEES 24 hours after extubation was 66.7%, and those exhibiting laryngeal injury was 87.9%. The bivariate analysis revealed a significant correlation between the number of comorbidities, intubation duration, laryngeal injury severity, and MPT value with the incidence of PED in the RSCM ICU. Moreover, the multivariate analysis showed that the duration of intubation exceeding 24 hours had a statistically significant association with the incidence of PED (p=0.003; OR 15.30; 95% CI 2.46-95.19).
Conclusion
The proportion of mild to severe dysphagia in post-extubation patients in the RSCM ICU is quite high. Intubation duration exceeding 24 hours and having more than one comorbidity significantly contribute to the increased risk of dysphagia in post-extubated patients in the RSCM ICU.
Introduction
Dysphagia is a clinical challenge that is often encountered in post-extubation patients in the intensive care unit (ICU), but this condition is still under-recognized. Globally, there are 13-20 million critically ill patients intubated in ICUs each year, but the exact incidence of post-extubation dysphagia (PED) is unknown [1-4]. Various risk factors for PED have been studied, including patient demographic factors, comorbidities, clinical diagnoses in the ICU, intubation-related factors, and others [4-7].
Screening and evaluation of PED can be done using videofluoroscopic swallow study (VFSS) and flexible endoscopic evaluation of swallowing (FEES). However, evaluation on ICU patients is carried out using FEES as it enables a comprehensive assessment of the pharyngeal stage of swallowing process, aiding in swallowing therapy to determine the appropriate diet and learn necessary swallowing maneuvers for the patient without transporting the patient to the fluoroscopy suite in radiology department [7,8].
Dysphagia has serious impacts on the patients and the health care system. A 5-year longitudinal cohort study involving 13 ICUs at 4 US teaching hospitals revealed dysphagia symptoms persisted for more than 6 months in 23% of ICU patients after discharge from the hospital [9]. Moderate or severe dysphagia is often associated with an increased risk of reintubation, pneumonia, a longer hospital stay, reduced food intake, prolonged nasogastric tube use, and an increased mortality risk [2,7,10].
This study aims to identify the proportion of PED through FEES examination and factors associated with PED in the RSUPN Dr. Cipto Mangunkusumo (RSCM) ICU, Jakarta, Indonesia. By investigating these factors, we seek to enhance our understanding of PED and improve patient outcomes through targeted interventions and management.
Subjects and Methods
This two-stage study was conducted in the ICU and ENT bronchoesophagology polyclinic of RSCM from November 2022 to January 2023. The first stage involved a cross-sectional study where FEES examinations were performed on post-extubation patients in the RSCM ICU. Internal comparisons were made regarding the patient’s demographic and clinical characteristics intubation-related factors, degree of laryngeal injury, and maximum phonation time (MPT) value on the incidence of dysphagia. The second stage was a pre-post study on subjects with dysphagia to evaluate the proportion of persistent dysphagia through FEES examination 72 hours post-extubation.
Non-probability sampling using consecutive sampling was employed. Inclusion criteria included: patients aged >18 years, ICU patients with intubation time >12 hours and extubated within the first 24 hours, cooperative, fully conscious, able to sit at a minimum of 45 degrees, and willing. Exclusion criteria encompassed unwillingness to participate, agitation, Glasglow Coma Scale <14, unstable cardiopulmonary condition (such as bradycardia or severe shortness of breath), risk or presence of bleeding in upper aerodigestive area, platelets <50,000, history of dysphagia, tracheostomy, or fasting due to medical reasons.
Statistical analysis
Data analysis was performed using SPSS version 20.0 software (IBM Corp., Armonk, NY, USA). To measure the distribution of demographic and clinical characteristics of patients, factors related to intubation, and MPT values, and to determine the picture of dysphagia in post-extubation patients based on the distribution of FEES parameters, a univariate test analysis was carried out. Ordinal and nominal data are presented in the form of frequency distributions and percentages. Numerical data were tested for normality using the ShapiroWilk method. Data with a normal distribution are presented in the form of a mean and a standard deviation. Data with a non-normal distribution are presented in the form of the median and range. Chi-square or Fisher’s exact test was used to evaluate the relationship between two categorical variables with a 5% significance. To assess interactions between independent variables and confounders, if there is more than one variable that has a pvalue <0.25 on dysphagia complaints, it is included in a multivariate analysis using the logistic regression method.
Results
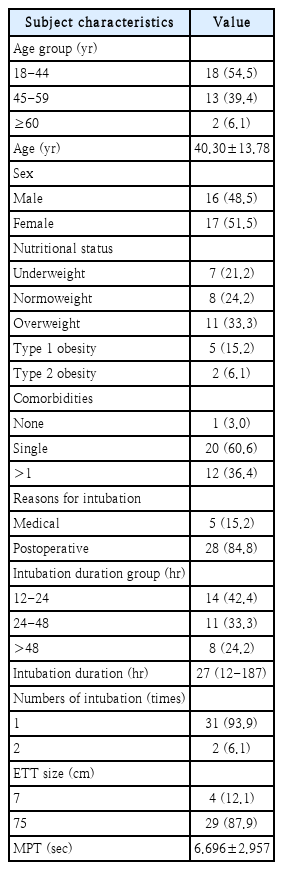
The study includes age, gender, nutritional status, comorbidities, intubation reason, duration, number, endotracheal tube (ETT) size, and MPT for basic characteristics. Characteristic data are presented in Table 1.
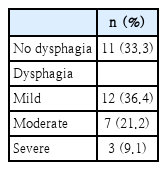
Based on initial FEES examination (24 hours post-extubation), the diagnosis of dysphagia was obtained in 22 of 33 subjects (66.7%), with mild dysphagia in 12 (36.4%), moderate in 7 (21.2%), and severe in 3 (9.1%) (Table 2). Based on Warnecke, et al. [11] classification, mild dysphagia is diagnosed when preswallowing leakage and residue was present without penetration and aspiration. Moderate dysphagia is diagnosed when penetration and/or aspiration is present on one type of food consistency. Moreover, severe dysphagia in diagnosed when penetration and/or aspiration is present on more than two types of food consistency [12].
Based on the initial FEES examination, laryngeal injury was obtained by 29 of 33 subjects (87.9%), with mild injury in 11 (33.3%), moderate in 12 (36.4%), and severe in 6 (18.2%).
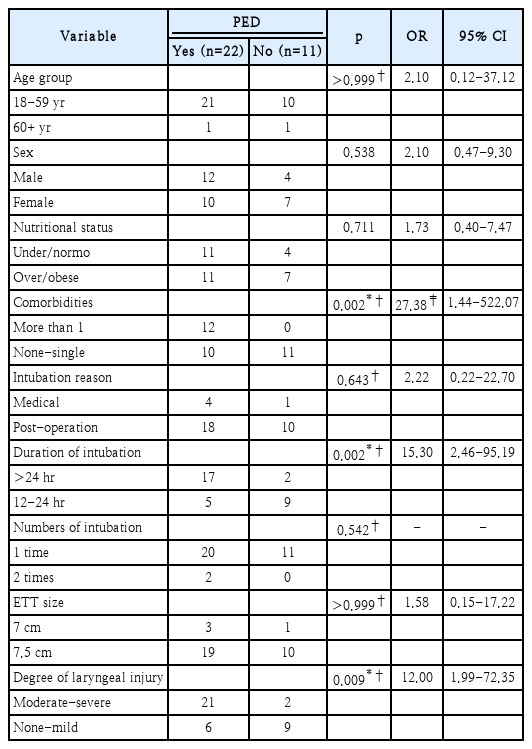
In this study, factors associated with the PED incidence from the initial FEES were analyzed using bivariate and multivariate logistic regression analysis. Results in Table 3 show a significant relationship between PED and the number of comorbidities, duration of intubation, and laryngeal injury degree (p<0.05).
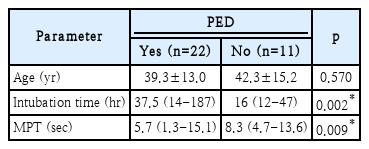
A bivariate analysis of PED status based on parameters of age, length of intubation, and MPT showed that there was a significant difference in the median value of length of intubation and MPT value with the incidence of PED (p<0.05) (Table 4).
Based on the multivariate logistic regression analysis in Table 5, the probability of dysphagia for an intubation duration of 12-24 hours is 35.71%, while for >24 hours, can reach 89.47%. The incidence ranges from mild to severe dysphagia.
Subjects with dysphagia had a second FEES examination at 72 hours post-extubation, aimed to detect persistent dysphagia. In this examination, 11 of 22 study subjects (50%) had persistent dysphagia with over half (8/11) having mild, 2 moderate, and 1 severe dysphagia initially.
Discussion
This study reveals that 66.7% of the 33 subjects treated in the RSCM ICU experienced PED, as determined by their first FEES examination. The overall rates of PED in this study are higher than those reported in the systematic review conducted by Skoretz, et al. [3], which included 3520 subjects and reported a rate of 62%. Similarly, McIntyre, et al. [13] reported a rate of 41% in a larger population. Both studies utilized a range of subjective and objective techniques to assess dysphagia, including the use of FEES. The variation in prevalence observed in comparison to previous studies can be attributed to disparities in population demographics, study methodology, diagnostic criteria for dysphagia, timing of diagnosis, and the specific instruments employed for dysphagia diagnosis. The study population in this research was more diverse than in previous studies, both in terms of age and the presence of other medical conditions. This study employs FEES as the benchmark for diagnosing dysphagia, thus exerting a significant impact on the results, which indicate a higher prevalence of dysphagia compared to alternative subjective examination methods. Most previous studies used aspiration as a determinant of dysphagia, possibly because aspiration is a major cause of nosocomial infections in critically ill patients. In this study, we did not limit the definition of dysphagia to penetration or aspiration only but also based on the findings of preswallowing leakage and residue which was considered mild dysphagia.
The initial FEES results indicated that nearly all participants (87.9%) exhibited laryngeal injuries in this study. Research conducted by Shinn, et al. [14], reported a prevalence of laryngeal injury of 57% in individuals who underwent intubation for a duration exceeding 12 hours. The disparity arises from the fact that the examination conducted in that study involved a video laryngoscopy at 36 hours post-extubation, in contrast to our study which performed a laryngeal evaluation at 24 hours post-extubation. Furthermore, that study did not consider erythema and edema as immediate laryngeal injuries. The elevated incidence of laryngeal injuries could potentially be attributed to pre-existing laryngeal diseases or abnormalities, as these were not specifically excluded during the recruitment phase of the study subjects. This variable has the potential to be a complicating factor in the research findings, which cannot be definitively excluded at this time.
The process of aging impacts the ability to swallow by causing physiological changes, alterations in sensory perception, and a reduction in the reflexes that protect the airway. The study conducted by Bordon, et al. [15] revealed individuals aged 55 and above have a 2.5-fold greater likelihood of experiencing PED compared to younger individuals. This study found no statistically significant correlation between age and the occurrence of PED. This could be attributed to the limited sample size of elderly participants, specifically only two subjects. However, the study did reveal that one out of the two elderly subjects exhibited moderate dysphagia.
The number of subject genders is relatively almost the same between males and females. The incidence of PED was found to be independent of gender. This finding aligns with prior research, which indicated that laryngeal injuries in individuals after extubation were equally distributed among both genders. Therefore, gender cannot serve as a clinical indicator for assessing dysphagia [16].
The findings of this study indicate a lack of correlation between nutritional status and the occurrence of PED. This discovery is in direct opposition to prior investigations. The study conducted by Sassi, et al. [17] revealed a strong correlation between individuals with a higher body mass index (BMI) and the occurrence of dysphagia. According to the research conducted by Yoo, et al. [18], reports that BMI is not associated with increased mortality in PED patients.
This study reports a significant relationship between the number of comorbidities and the incidence of PED (p=0.002). All subjects who had more than one comorbidity were found to have PED. Critically ill patients in the ICU have various comorbid diseases that can influence the incidence of dysphagia. Factors that influence breathing patterns, such as chronic respiratory disease, can affect the coordination of breathing and swallowing. Hypertension and diabetes increase the susceptibility of individuals to develop PED by promoting the occurrence of nerve damage caused by diabetes and atherosclerosis in various arteries, including those located in the larynx [19].
The study revealed no significant correlation between the cause of intubation and the presence of PED. This aligns with research indicating that medical and post-operative factors for intubation do not definitively indicate the presence or absence of PED [20].
This study revealed no correlation between the frequency of intubations and the occurrence of PED. This can be explained by the limited number of subjects who underwent multiple intubations (6.1%) in this study. Barquist, et al.’s [5] research also yields comparable findings.
Research by Krisciunas, et al. [6] reported that the relationship between ETT and the incidence of dysphagia based on aspiration was more significant when compared between sizes 7.5 and 8.0. Based on these results, it can be considered that a smaller ETT size has better benefits against laryngeal pathology and post-extubation aspiration. In this study, ETT size did not have a significant relationship with the incidence of PED. This may be influenced by the ETT sizes used in this study being only 7.0 and 7.5.
In this study, a significant relationship was found between moderate-severe laryngeal injury and the incidence of PED. This is in accordance with several previous studies [6,21]. It is known that a patient’s susceptibility to laryngeal injury depends on the anatomical structure, size of the ETT, and length of exposure to the ETT [22].
This study reported subjects with PED had shorter MPT values with a median value of 5.7 (min 1.3-max 15.1) and subjects without dysphagia with a median value of 8.3 (4.7-13.6), p=0.009. These findings support findings by Ko, et al. [23] who reported an association between MPT and swallowing-related elements with swallowing function and phonation in patients with Parkinsonism. The MPT value is related to oropharyngeal motor function, such as tongue movement (bolus formation, oral transit time), laryngeal elevation, and pharyngeal swallowing reflex [23].
This study found that an intubation duration of >24 hours had a 15 times greater risk of PED events compared to research subjects with an intubation duration of <24 hours (p<0.05). This finding is in line with previous research by Kim, et al. [24] which reported that patients with a longer duration of intubation had a higher risk of post-extubation aspiration by 1.09 times (95% CI 1.01-1.18; p<0.05). So the length of intubation can be useful for identifying patients who require postextubation swallowing evaluation [24].
The multivariate logistic regression analysis equation in this study indicates that there is a 35.71% probability of experiencing mild-severe dysphagia during intubation for 12-24 hours. However, after 24 hours, the probability increases significantly to 89.47%. These findings indicate that dysphagia can manifest after a brief period of intubation. Therefore, it is crucial to conduct a thorough assessment and implement suitable measures to mitigate the risk of additional dysphagia leading to aspiration and pneumonia.
The study discovered that 50% of individuals experienced ongoing dysphagia 72 hours after extubation. A systematic review by Kelly, et al. [25] found the prevalence of persistent dysphagia at 23%. These outcomes were measured using a combination of instrumental and non-instrumental assessments carried out at 12-240 weeks -post-extubation. This is different from the results of this study because the assessment was carried out at 72 hours post-extubation. Persistent dysphagia, as discovered by Macht, et al. [10], is linked to unfavorable outcomes, particularly moderate-severe dysphagia. Additionally, this study revealed that up to 50% of individuals with PED encountered spontaneous improvement. This finding provides evidence that the swallowing function can experience rapid improvement following extubation.
In conclusion, intubation duration exceeding 24 hours and number of comorbidities more than 1 are the most significant autonomous risk factors for PED, presenting a 15-fold risk. Conversely, age, sex, nutritional status, reason for intubation, number of intubations, and ETT size, show no correlation with PED risk. However, our study has insufficient sample size. Future studies should be conducted with more subjects to get a better conclusion regarding the proportion and factors associated outcome on PED.
Acknowledgements
Our study has received approval from the Ethics Committee of the Faculty of Medicine Universitas Indonesia and permission to do the research from Cipto Mangunkusumo General Hospital. Informed consent has been obtained from each patient before the initiation of data collection.
Notes
Author contributions
Conceptualization: Susyana Tamin. Data curation: Indira Sari. Formal analysis: Syahrial M. Hutauruk. Investigation: Susyana Tamin. Methodology: Elvie Zulka Kautzia Rachmawati. Project administration: Indira Sari. Resources: Dita Aditianingsih. Supervision: Fauziah Fardizza. Validation: Joedo Prihartono. Writing—original draft: Indira Sari. Writing—review & editing: Susyana Tamin.