 |
 |
AbstractBackground and Objectives Appropriate diagnostics help in determining the best approach for managing adenoid hypertrophy. This study aimed to learn more about many diagnostic procedures for adenoid hypertrophy to improve good health and the quality of medical decisions, such as clinical symptoms measured by clinical scores, radiological examination, and nasopharyngeal endoscopy.
Subjects and Method An examination was conducted on 73 patients who had symptoms of adenoid hypertrophy at the Otorhinolaryngology-Head and Neck Surgery (ORL-HNS) outpatient unit. The participants underwent all of the diagnostic stages, including history taking and physical examination to determine the clinical scores, radiological examination, and the endoscopic examination of the nasopharynx. The correlation between the clinical scores, radiological examination, and the endoscopic examination of the nasopharynx was statistically analyzed.
Results Of the 73 patients, 46 were male (63%) and 27 were female (37%). The correlation between each examination modality was determined using the Spearman’s statistical analysis. There was a moderately strong correlation between clinical scores and radiological examinations with the p-value of 0.0022 and the r-value of 0.3529, and a very strong significant correlation between the clinical scores and endoscopic examination with the p-value of 0.0001 and the r-value of 0.7562. In comparison, the correlation between the radiological and endoscopic examinations of the nasopharynx was significant but weak, with the p-value of 0.0057 and the r-value of 0.3208.
Conclusion The findings indicated that radiological and endoscopic examinations of the nasopharynx could be used to establish a correlation between adenoid hypertrophy and clinical symptoms associated with adenoid hypertrophy. Although the correlation strength was statistically different, these diagnostic modalities can complement each other.
IntroductionAdenoids are part of the ring of waldeyer and have a role in the body’s defense function [1,2]. Symptoms of adenoid hypertrophy include rinolalia occlusal, mouth open to breathe, adenoid face, nasal aprosexia, headache, runny nose, chronic cough, decreased appetite, and reduced hearing. The adenoids become hypertrophied in pathological conditions that often occur in children, which can cause complications in nasal obstruction, snoring, sleep apnea, otitis media, and affect the craniofacial shape. Adenoid hypertrophy management with medication or requires an adenoidectomy. Indications for adenoidectomy include chronic infection and obstructive airways caused [3,4]. The choice to undergo adenoidectomy should be carefully, even if the consequences of post-adenoidectomy on the immune system are still debatable [5-8].
The decision to refer for adenoidectomy must be based on clinical aspects, physical examination, and supporting tests [3,9]. The clinical aspect is important for patient [10]. Clinical aspects include history taking and physical examination, which may be quantified using questionnaires, clinical scores, and nasal obstruction evaluation [11]. However, an objective investigation must support this value to determine the exact degree of adenoid hypertrophy [6,12]. Adenoids in the nasopharynx are difficult to see, so size evaluation to determine the degree of obstruction caused becomes a challenge. Several methods are available for assessing the adenoids’ size, including posterior rhinoscopy, acoustic rhinometry, rhinomanometry, lateral cervical x-ray, and nasopharyngscopy. Nasopharyngscopy and radiological examination are the most frequently used modalities in clinical practice [12-14].
Radiological examinations have long been used to diagnose adenoid size. This examination is simple, easy to perform, and reproducible. Weaknesses in the radiological examination are caused by various factors, including anatomical changes caused by patient movement, particularly in children, patient breathing movements, radiation exposure, and the interpretation and visualization of results in the form of two-dimensional images that do not adequately represent the adenoids’ condition [15]. Another method for evaluating adenoids is nasopharyngscopy, the gold standard for examining adenoid hypertrophy, but not all health facilities have it. Nasopharyngscopy provides direct visualization of the adenoid size. Weaknesses of nasopharyngscopy are subjective and influenced by the examiner’s skill, and are challenging to perform because pediatric patients are often not cooperative [16-19].
Each modality of diagnostic support for adenoid examination has advantages and disadvantages [13]. So, there is a need to research developing a clinical-based diagnostic of adenoid hypertrophy and supplementary examination as an objective examination. This study aimed to determine the correlation between the clinical score of adenoid hypertrophy and radiological and nasopharyngscopy examination results. The results of this study can be used as a guide for general practitioners in primary care to decide whether a patient’s referral to a health facility requires further action and a guide for an Otorhinolaryngology-Head and Neck Surgery (ORL-HNS) specialist to decide on an adenoidectomy based on the clinical, radiological, or nasopharyngoscopy so good health and quality of medical decisions can be improved.
Subjects and MethodsThe study involved 73 patients from January 2019-June 2021 with symptoms of adenoid hypertrophy. The study exclusion factors were patients with obstruction due to deviated septum, rhinosinusitis, uncontrolled allergic rhinitis, patients who had undergone adenoidectomy, large tonsils T2-T4, or acute infections nose, palate, or nasopharynx.
The patient underwent history taking through heteroanamnesis and clinical examination, lateral cervical x-ray, and nasopharyngscopy to determine the size of the adenoids. Clinical scores, radiographic examination, and nasopharyngeal endoscopic examinations were all done by separate doctors who were blinded to the findings of the other investigations. The Research Ethics Comittee of Universitas Airlangga Acedemic Hospital accepted the study protocol with reference number 190/KEP/2020, and the parents provided informed consent.
Clinical assessment of patients using clinical scores that have been validated by Sharifkashani, et al. [6]. The clinical score assessment used was signs and symptoms of airway obstruction caused by adenoid hypertrophy, including difficulty breathing during sleep/dyspnea (D), apnea (A), and snoring (S). The scores were determined using the criteria listed in Table 1. The final score was calculated as the function of the three factors listed below: 1.42D + 1.41A + 0.71S - 3.83 (Table 1). Patients were then categorized into the mild category if the score <-1, moderate category if the score was -1 to 3.5, and severe category if the score was >3.5 (Table 2). The clinical score examination was performed by an ORL-HNS specialist blindly. The clinical score examination was carried out by one certified ORL-HNS doctor, while another certified ORL-HNS doctor carried out the endoscopy examination. The two doctors did not know each other’s examination results to ensure the blindness and objectivity of this study.
A lateral cervical x-ray was used to obtain a two-dimensional image of the adenoid’s size compared to the nasopharynx. The patient lies on the examination table in a semi-prone or sitting position. The patient’s head is positioned true lateral and attached to the bucky, infra-orbitomeatal line parallel to the horizontal plane of the cassette. Mouth open as wide as possible. Central X-Ray is perpendicular to the plane of the cassette. Center point ±2 cm below MAE with 100 cm film-focus distance. Set the exposure limit as needed. Instruct the patient not to move during the x-ray to avoid repeating the photo. According to the Cohen and Konak method, the following categories of adenoid hypertrophy exist category 1, 2, 3 (Table 2) [6]. Radiology results are read blindly by the radiologist. There was only one radiologist involved in this study, the radiologist did not know the results of the examinations from other doctors to ensure the blindness and objectivity of this study.
Patients underwent nasopharyngoscopy using a rigid endoscope measuring 2.7 mm in diameter with a 0-degree telescope made by the German company Karl Storz. The examination was conducted at the ORL-HNS outpatient unit. Local anesthesia with lidocaine and phenylephrine was administered before the examination, and sedation was used if the child was uncooperative. The endoscopic examination’s findings were categorized according to the degree of obstruction caused by hypertrophic adenoids covering the choana. According to the Clemens and McMurray criteria, adenoids were classified as grades 1, 2, 3, and 4 (Table 2). An ORL-HNS expert blindly read the radiological findings. A radiologist read the x-ray examination, then the conclusion of the radiological findings was read by the ORL-HNS doctor. Clinical assessment, x-ray, and endoscopy were not performed simultaneously on the same day.
For statistical analysis, the GraphPad Prism software version 8 was utilized. Spearman’s correlation coefficient was used to compare pairings of the four categories. Statistical significance was defined as a p-value <0.05.
ResultsThe study sample consisted of 73 patients with symptoms of adenoid hypertrophy. Sex showed that there were 46 males (63%) and 27 females (37%). The mean age is 8.945±3.055 years. The youngest is one year, and the oldest is 14 years. The results of the clinical examination score obtained an average value of 1.918±0.7022. The results of the radiological examination score obtained an average value of 1.521±0.5299 (Fig. 1). The results of the endoscopic examination score obtained a mean value of 2.151±0.7578 (Fig. 2). Thirty-six patients (49%) had adenoidectomy, whereas 37 patients (51%) did not (Table 3). The decision to perform adenoidectomy was considered in patients with clinical scores, radiology scores, and endoscopy scores 2 and 3.
Correlations between age, clinical score, radiological score, and endoscopic score were determined using statistical tests. The homogeneity test was carried out with the Kolmogorov-Smirnov test. The homogeneity test revealed that the data were not normally distributed, necessitating the application of the Spearman correlation test.
Correlation of age with clinical scores found a significant correlation (p=0.0015) between age and clinical scores with a moderate degree of negative correlation (r=-0.3644) which means that the younger the patient, the higher the clinical score. The correlation between age and cervical lateral x-ray radiological scores showed no significant correlation (p=0.7519), and the strength of the negative correlation was very weak (r=-0.03764). Meanwhile, the correlation between age and endoscopic scores was found to be significant (p=0.0003) with a moderate degree of negative correlation (r=-0.4144), which means that the younger the patient, the higher the endoscopy score (Table 4).
The correlation of clinical scores with radiological scores of lateral cervical x-ray obtained significant results (p=0.0022) with a moderate correlation coefficient (r=0.3529). Correlation of clinical scores with endoscopic scores obtained a significant correlation (p<0.0001) with a strong correlation (r=0.7562) which means the higher the clinical score, the higher the endoscopy score (Table 4). Correlation of lateral cervical x-ray radiology scores with endoscopic scores found a significant correlation (p=0.0057) with a moderate level of correlation (r=0.3208) (Table 4).
DiscussionAdenoids are a vital part of the Waldeyer ring in the nasopharynx, an essential function in the immune system [13]. Adenoids may hypertrophy from the age of two years, undergo hyperplasia between the ages of three and eight years, and play a critical function in the immune system between three and ten years. After the age of eight years, the adenoids maintain a reasonably consistent size. After puberty, adenoids undergo adenoid involution [18]. This research discovered most instances between the ages of 6-10 years, 41 patients (56%), and a negative correlation between patient age and adenoid hypertrophy, meaning that the older the kid, the smaller the adenoid enlargement [20]. Allergic rhinitis, chronic illness, environmental exposure, and allergies may contribute to adenoid hypertrophy in adulthood [21]. Hypertrophic adenoids may block the choana, disrupt the flow of respiratory air from the nose to the lungs, obstruct the drainage of secretions from the nasal cavity, sinuses, and ears, and serve as a reservoir for bacterial pathogens to proliferate quickly after viral infection [4,22].
Adenoid hypertrophy associated with complications necessitates adenoidectomy. Adenoidectomy is one of the most frequently performed surgical operations on children. Although the indications for adenoidectomy are still debatable due to the function of adenoids in the immune system, it should perform if it causes obstructions of the upper airway [3]. Therefore, it is essential to investigate clinical symptoms of adenoid hypertrophy during the examination, particularly to establish a diagnosis of adenoid hypertrophy and its associated complications [6,9,23]. This research assessed airway obstruction using a clinical score of adenoid hypertrophy since airway obstruction is the primary reason for adenoidectomy. There were 15 patients (20%) with severe clinical scores and 37 patients (51%) with intermediate clinical scores for symptoms of airway obstruction, making these individuals the primary candidates for adenoidectomy. Clinical ratings alone, however, are insufficient to make a definitive decision on adenoidectomy. Therefore, an objective investigation is needed [3].
The objective examination recommended is lateral cervical x-ray and nasopharyngoscopy of the nasopharynx to reach the adenoids in the nasopharynx. Several studies were conducted to assess the efficacy of these examination modalities [11,13,24]. This research study looks for the correlation between clinical scores, lateral cervical x-ray, and nasopharyngoscopy so that an objective examination can support the subjective clinical aspects as a material for adenoidectomy decisions.
This research study found that clinical scores and radiological examinations of lateral cervical x-ray were significant with moderate strength (p=0.0022 and r=0.3529). The results of this study are the same as those conducted by Saedi, et al. [13] in 2011, and Dixit and Tripathi [9] in 2016 found a significant relationship. However, there are also research studies, among others, by Sharifkashani, et al. [6] in 2015, Kugelman, et al. [23] in 2019, and Jyothirmai, et al. [11] in 2020 stated that there was no significant relationship between the clinical score of adenoid hypertrophy and the results of lateral cervical x-ray. Variations in endoscopic examination results occur because the patients examined are patients with various levels of clinical symptoms (clinical scores). Not only in patients who have a high clinical score alone. So that with the differences in the results of lateral cervical x-rays, it can still be used as a screening tool in determining the need for follow-up treatment of adenoid hypertrophy [1]. Methods of reading the results of radiological examinations include the Fujioka, Young, and Girdany method or commonly called the adenoid nasopharyngeal ratio. Another method is the Cohen and Konak method. The disadvantages of radiological examination are that it only provides a two-dimensional picture, superimposition of anatomical structures can occur, and radiation exposure [5,15].
Nasopharyngscopy is recommended as the gold standard for diagnosing adenoid hypertrophy because it provides a direct view of the adenoids [12]. However, nasopharyngoscopy is influenced by the subjectivity and skill of the examiner. Nasopharyngoscopy is invasive and is quite difficult to perform in children so sometimes sedation is required for nasopharyngoscopiy procedures [16]. This study found a significant correlation with a very strong degree of association between clinical scores and nasopharyngoscopy examination scores (p<0.0001, r=0.7562). A study conducted by Saedi, et al. [13] in 2011, Sharifkashani, et al. [6] in 2015, and Kugelman, et al. [23] in 2019 gave the same result, namely that there was a significant correlation between clinical scores and the results of nasopharyngoscopy.
Many researchers have correlated lateral cervical x-ray and nasopharyngoscopy. Several studies have stated a significant correlation between radiological examinations and endoscopic examinations, including Saedi, et al. [13] in 2011, Lertsburapa, et al. [7] in 2010, Kurien, et al. [15] in 2005, Dawood and Khammas [24] in 2017, Hamza, et al. [25] in 2019; Harugop, et al. [12] in 2020. While the study conducted by Feres, et al. [1] in 2014 and Jyothirmai, et al. [11] in 2020 stated a weak relationship between radiological and endoscopic examinations. Research states there is no relationship between lateral cervical x-ray radiological examinations with nasopharyngeal endoscopy, among others, by Sharifkashani, et al. [6] in 2015. This study showed a correlation between lateral cervical x-ray and nasopharyngoscopy examination, but the correlation was weak (p=0.0057 and r=0.3208).
Nasopharyngoscopy is more recommended than lateral cervical x-ray in establishing the diagnosis of adenoid hypertrophy, especially to deciding on adenoidectomy [11,12,15,24]. The decision on adenoidectomy should be based on the gold standard examination, namely nasopharyngoscopy so that the procedure is carried out according to the indications and avoid mistakes in deciding on adenoidectomy [3,7,10,16]. The decision on adenoidectomy should be based on clinical considerations supported by supplementary examination. In this research study, clinical examination supported by objective examination used a radiological examination of lateral cervical x-ray and endoscopic examination. Patients with severe clinical symptoms (score 3) were found in 27 patients (37%) and moderate clinical symptoms in 30 patients (41%). Adenoidectomy was performed in 36 patients (49%). The decision for adenoidectomy took into account the clinical aspects, the results of the radiological examination of the lateral cervical x-ray, and the results of the nasopharyngoscopy.
Clinical examination can be used as a screening tool for adenoid hypertrophy and further management [6,11,25]. Based on the studies’ results, developing a clinical score as an initial screening for adenoid hypertrophy is necessary. The modalities of clinical examination, radiological examination, and endoscopic examination can complement each other and be adapted to the facilities available in health services [6,9,13].
In conclusions, nasopharyngoscopy is the gold standard for diagnosing adenoid hypertrophy. Radiological examination of lateral cervical x-ray can also be used to confirm the diagnosis of adenoid hypertrophy. The clinical score of adenoid hypertrophy can be used as a diagnostic screening tool to determine further adenoid hypertrophy management. The decision to perform adenoidectomy should be based on clinical aspects and objective examination. The recommended objective examination is nasopharyngscopy. If there is no nasopharyngscopy, a lateral cervical x-ray can still be used.
ACKNOWLEDGMENTSWe thank all patients for their kind cooperation. Thank Universitas Airlangga and Universitas Airlangga Academic Hospital, who have supported this research to guide the management of adenoid hypertrophy.
NotesAuthor Contribution Conceptualization: Puguh Setyo Nugroho, Rosa Falerina, Hendra Kurnia Rakhma. Data curation: Puguh Setyo Nugroho, Rosa Falerina, Hendra Kurnia Rakhma. Formal analysis: all authors. Funding acquisition: all authros. Investigation: Puguh Setyo Nugroho, Rosa Falerina, Hendra Kurnia Rakhma. Methodology: all authors. Project administration: Puguh Setyo Nugroho, Rosa Falerina, Hendra Kurnia Rakhma. Resources: Puguh Setyo Nugroho, Rosa Falerina, Hendra Kurnia Rakhma. Software: all authors. Supervision: Puguh Setyo Nugroho, Rosa Falerina, Hendra Kurnia Rakhma. Validation: all authors. Visualization: all authors. Writing—original draft: Puguh Setyo Nugroho, Rosa Falerina, Hendra Kurnia Rakhma. Writing—review & editing: Puguh Setyo Nugroho, Alfian Nurfaizi. Fig. 1.Radiological examination without adenoid enlargement and adenoid enlargement grade I, II, and III. A: No adenoid enlargement. B: Adenoid enlargement grade I (0%–50% of the nasopharynx is filled). C: Adenoid enlargement grade II (50%–75% of the nasopharynx is filled tissue). D: Adenoid enlargement grade III (75%–100% of the nasopharynx is filled). 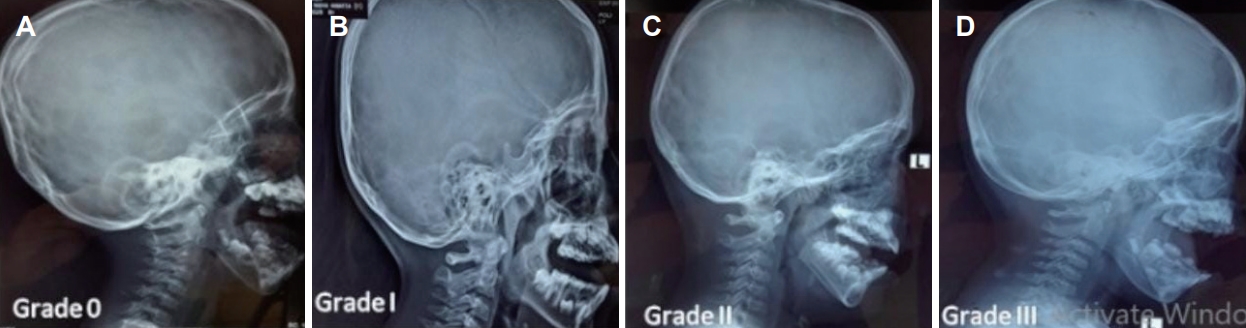
Fig. 2.Endoscopic examination of the nasopharynx without adenoid enlargement and adenoid enlargement grade I, II, and III. A: No adenoid enlargement. B: Adenoid enlargement grade I (≤1/3 of the choana). C: Adenoid enlargement grade II (1/3–2/3 of the choana). D: Adenoid enlargement grade III (≥2/3 of the choana/nearly obstruction). 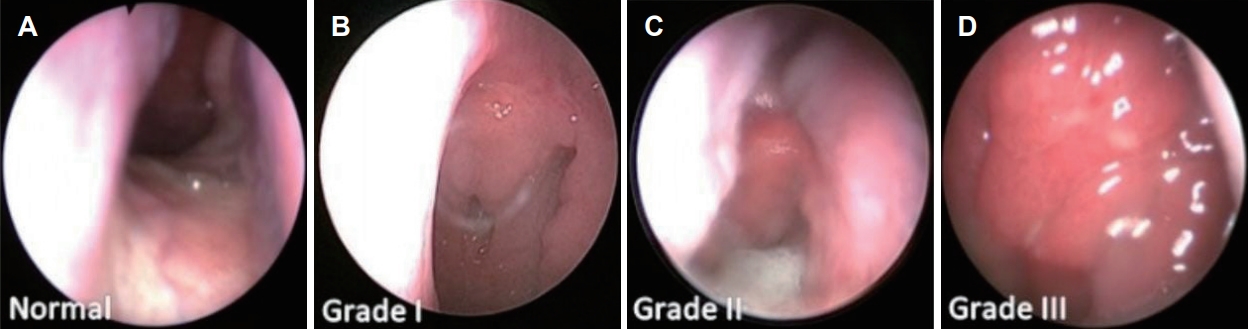
Table 1.Assessment of the patient’s clinical score
Table 2.Clinical, radiological, and endoscopic assessment score Table 3.Research samples and examination results (n=73) Table 4.Correlation of adenoid hypertrophy with various examination modalities (n=73) REFERENCES1. Feres MF, Hermann JS, Sallum AC, Pignatari SS. Radiographic adenoid evaluation: Suggestion of referral parameters. J Pediatr (Rio J) 2014;90(3):279-85.
2. Casteleyn C, Breugelmans S, Simoens P, Van den Broeck W. The tonsils revisited: Review of the anatomical localization and histological characteristics of the tonsils of domestic and laboratory animals. Clin Dev Immunol 2011;2011:472460.
3. Baddour HM, Statham MM. Tonsillectomy and adenoidectomy. In: Lubin MF, Dodson TF, Winawer NH, eds. Medical Management of the Surgical Patient: A Textbook of Perioperative Medicine. 5th ed. Cambridge, UK: Cambridge University Press; 2013. p. 758-60.
4. Pereira L, Monyror J, Almeida FT, Almeida FR, Guerra E, FloresMir C, et al. Prevalence of adenoid hypertrophy: A systematic review and meta-analysis. Sleep Med Rev 2018;38:101-12.
5. Caylakli F, Hizal E, Yilmaz I, Yilmazer C. Correlation between adenoid-nasopharynx ratio and endoscopic examination of adenoid hypertrophy: A blind, prospective clinical study. Int J Pediatr Otorhinolaryngol 2009;73(11):1532-5.
6. Sharifkashani S, Dabirmoghaddam P, Kheirkhah M, Hosseinzadehnik R. A new clinical scoring system for adenoid hypertrophy in children. Iran J Otorhinolaryngol 2015;27(78):55-61.
7. Lertsburapa K, Schroeder JW Jr, Sullivan C. Assessment of adenoid size: A comparison of lateral radiographic measurements, radiologist assessment, and nasal endoscopy. Int J Pediatr Otorhinolaryngol 2010;74(11):1281-5.
8. Dibildox J, Bowen AD. Impact of adenotonsillectomy on the immune system. In: Sih T, Chinski A, Eavey R, Godinho R, eds. XIII IAPO Manual of Pediatric Otorhinolaryngology. São Paulo, Brazil: Interamerican Association of Pediatric Otorhinolaryngology; 2014. p. 91-9.
9. Dixit Y, Tripathi PS. Community level evaluation of adenoid hypertrophy on the basis of symptom scoring and its X-ray correlation. J Family Med Prim Care 2016;5(4):789-91.
10. Babakurban ST, Aydin E. Adenoidectomy: Current approaches and review of the literature. Turkish J Ear Nose Throat 2016;26(3):181-90.
11. Jyothirmai ASL, Sadhana O, Chandra TS, Murthy PSN. Assessment of adenoid hypertrophy with clinical grading versus radiology and endoscopy: A cross-sectional study. IP J Otorhinolaryngol Allied Sci 2020;3(4):130-5.
12. Harugop AS, Soni S, Tejaswini JS. Efficacy of nasoendoscopy over X-ray nasopharynx in diagnosing adenoid hypertrophy. Acta Scientific Otolaryngology 2020;2(7):19-24.
13. Saedi B, Sadeghi M, Mojtahed M, Mahboubi H. Diagnostic efficacy of different methods in the assessment of adenoid hypertrophy. Am J Otolaryngol 2011;32(2):147-51.
14. Cho JH, Lee DH, Lee NS, Won YS, Yoon HR, Suh BD. Size assessment of adenoid and nasopharyngeal airway by acoustic rhinometry in children. J Laryngol Otol 1999;113(10):899-905.
15. Kurien M, Lepcha A, Mathew J, Ali A, Jeyaseelan L. X-Rays in the evaluation of adenoid hypertrophy: It’s role in the endoscopic era. Indian J Otolaryngol Head Neck Surg 2005;57(1):45-7.
16. Pagella F, Pusateri A, Chu F, Cairello F, Benazzo M, Matti E, et al. Adenoid assessment in paediatric patients: The role of flexible nasal endoscopy. Int J Immunopathol Pharmacol 2011;24(4_Suppl):49-54.
17. Parikh SR, Coronel M, Lee JJ, Brown SM. Validation of a new grading system for endoscopic examination of adenoid hypertrophy. Otolaryngol Head Neck Surg 2006;135(5):684-7.
18. Kubba H, Bingham BJ. Endoscopy in the assessment of children with nasal obstruction. J Laryngol Otol 2001;115(5):380-4.
19. Kindermann CA, Roithmann R, Lubianca Neto JF. Sensitivity and specificity of nasal flexible fiberoptic endoscopy in the diagnosis of adenoid hypertrophy in children. Int J Pediatr Otorhinolaryngol 2008;72(1):63-7.
20. Yonis MAM, Ibrahim MA, Farag FK, El Shennawy AM. Relationship between adenoidal hypertrophy and allergic rhinitis in children. Egypt J Hosp Med 2019;74(1):94-102.
21. Althobaiti T, Hadaidi WA, Alghamdi ASA, Alghashmari KFJ, Hadaidi AA, Abd-Elrahman TM. Adenoid hypertrophy in adults: Causes and precipitating factors. IJMDC 2020;4(11):1792-6.
22. Abd-allatif M, Ibrahim H, Yehia S, Abd-Elwahab S, Raghib K. The effect of adenoid hypertrophy on intelligence quotient at preschool age. Al-Azhar Assiut Med J 2014;12(1):94-113.
23. Kugelman N, Ronen O, Stein N, Huberfeld O, Cohen-Kerem R. Adenoid obstruction assessment in children: Clinical evaluation versus endoscopy and radiography. Isr Med Assoc J 2019;21(6):376-80.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |