 |
 |
AbstractBackground and ObjectivesIn the present study, we evaluated the treatment results of hypopharyngeal squamous cell carcinoma (HPSCC) patients and analyzed the occurrence of secondary primary malignancies. Treatments were based on two different surgical modalities (conventional pharyngo-laryngectomy vs. transoral surgery). In addition, prognostic factors of the patients were evaluated.
Subjects and MethodWe analyzed medical data of 232 patients diagnosed with HPSCC and underwent surgery at our hospital from January 2006 to December 2019.
ResultsThe 5-year recurrence-free survival was 67.2% for the stage I-II group and 64.9% for the stage III-IV group. The 5-year disease-specific survival was 78.2% for the stage I-II group and 54.5% for the stage III-IV group. N classification was significantly correlated with disease relapse and patient mortality. Patient age, sex, perineural invasion, extranodal extension, initial tumor stage, and early recurrence (within 6 months) were significantly associated with successful salvage treatment. The two surgical modalities did not yield different oncological outcomes. Secondary primary malignancies occurred most frequently in the esophagus, with no observed inferior survival rate in patients with second malignancies.
IntroductionHypopharyngeal squamous cell carcinoma (HPSCC) is a rare and aggressive cancer that accounts for 3%-5% of all head and neck cancers [1]. It is known to have a poor prognosis because patients often visit the hospital at an advanced stage of the disease. Cervical lymph node metastasis and submucosal tumor invasion are common [2-4]. In addition, smoking-induced secondary primary malignancies are common, and concurrent medical illnesses and poor nutritional status are also linked to an unfavorable prognosis for patients with HPSCC [1].
Traditionally, HPSCC treatment involved surgery with adjuvant therapy, such as radiotherapy or concurrent chemoradiotherapy (CCRT). However, many patients experienced a decreased quality of life, including speech and swallowing difficulties after treatment [1,2]. In recent decades, there has been a shift toward non-surgical therapies, primarily CCRT, to preserve organ and function. Comparisons with surgical modalities have shown comparable loco-regional control rates [5]. Nonetheless, the high toxicity of CCRT can lead to xerostomia, mucositis, and delayed dysphagia due to tissue fibrosis, impacting the quality of life for many patients over an extended period [2,6,7].
Recent advancements in robot technology and endoscopic instruments have fueled active research in transoral surgery for HNSCC treatment. Studies have reported outcomes of transoral surgery and compared its oncological and functional results with conventional treatments [8-10]. In the case of advanced HPSCC, new therapies combining neoadjuvant chemotherapy (NAC) and transoral robotic surgery (TORS) have shown promising oncological and functional outcomes. However, limitations such as single-institution studies and retrospective designs introduce selection bias, and comprehensive investigations on HPSCC’s natural course, prognostic factors, and treatment results are lacking due to the low incidence of HPSCC [11]. In this study, we analyzed data from HPSCC patients treated at a single institution to investigate treatment results with different surgical modalities (conventional pharyngo-laryngectomy vs. transoral surgery±NAC), prognostic factors, and the impact of secondary primary malignancies on these patients.
Subjects and MethodsThe Institutional Review Board of Yonsei University approved this retrospective study (No. 3-2023-0227). From January 2006 to December 2019, the medical records of 232 patients who were diagnosed with HPSCC and underwent surgery at our hospital were examined. Among the subjects, 26 were excluded from the study for the following reasons: 1) curative treatment was not performed because distant metastases were discovered at the time of diagnosis; 2) subjects had histological types of cancer other than squamous cell carcinoma; 3) follow-up was not performed for a sufficient amount of time.
Patient information, such as age, sex, and smoking history, was gathered from medical records. Tumor stage was determined using the 8th American Joint Committee on Cancer (AJCC) system. Treatment modalities, recurrence, site of recurrence, and salvage treatment were investigated. Oncological and functional results were evaluated based on the patient’s condition at the last follow-up. Pathological details such as surgical margin status, lymphovascular invasion (LVI), perineural invasion (PNI), extranodal extension (ENE), and tumor size were examined. During the research period, disease recurrence was categorized as local, regional, or distant metastasis based on the site of recurrence. The period from the initial treatment to the discovery of disease relapse was defined as the recurrence period. Patient mortality during the study period and the cause of death were investigated. Patient survival was analyzed based on the data of recurrence and death.
Every patient enrolled in this study underwent surgical treatment with curative intent. For surgical methods, conventional pharyngo-laryngectomy or transoral surgery±NAC was performed. NAC was administered preoperatively for some T3/T4 stage or advanced staged patients to reduce tumor volume. The NAC regimen consisted of intravenous cisplatin (70 mg/m2) on day 1 and oral TS-1 (gimeracil 5.8 mg/m2, oteracil 19.6 mg/m2, and tegafur 20 mg/m2) on days 1-14, repeated every 21 days. The choice of surgical method was made after evaluating the tumor size and extent and discussing the advantages and disadvantages with the patient. Elective neck dissection was performed for N0 cases, while N+ cases underwent modified radical neck dissection. Adjuvant radiotherapy or CCRT was considered if postoperative pathological results showed positive/close margins, LVI, PNI, ENE, or T3-4 findings.
Patient personal information, clinical records, surgical pathology, recurrence informations (rate, date and cause), and death informations (rate, date and cause) were gathered and analyzed. Categorical variables of two independent groups were compared using the chi-square or Fisher’s exact test. An independent two-sample t-test was used to evaluate differences in continuous variables between two independent groups. Multivariate Cox proportional hazards regression model was used to simultaneously analyze the effect of factors on distant metastasis and survival. The Kaplan-Meier curve was used to analyze disease-free survival and a log-rank test was used to assess the survival outcomes. To compare the survival analysis of the two heterogenous groups, propensity score matching (PSM) analysis was performed. SPSS version 18.0 (SPSS, Chicago, IL, USA) was used for statistical analyses. Statistical significance was set at p<0.05.
ResultsClinical characteristicsA total of 206 HPSCC patients participated in this study. 195 were males (94.7%) and 11 were females (5.3%). The average age was 65.4 years (range, 38-88 years). Smoking history was present in 158 patients (76.7%), and 155 patients (75.2%) had a history of alcohol consumption. The primary tumor sites were the pyriform fossa in 152 patients (73.8%), the posterior pharyngeal wall in 43 patients (20.9%), and the postcricoid region in 11 patients (5.3%). T stage was as follows: T1 (n=38, 18.4%), T2 (n=69, 33.5%), T3 (n=51, 24.8%), and T4 (n=48, 23.3%). N stage was as follows: N0 (n=63, 30.6%), N1 (n=15, 7.3%), N2 (n=123, 59.7%), and N3 (n=5, 2.4%). Postoperatively, 146 patients (70.9%) had clear margins, while 60 patients (29.1%) had positive margins. LVI was observed in 73 patients (35.4%) and PNI in 40 patients (19.4%). ENE findings were observed in 91 patients (44.2%). NAC was administered before surgery to 65 patients (31.6%). After surgery, 52 patients (25.2%) received additional radiation treatment, and 90 patients (43.7%) received CCRT (Table 1).
Oncological resultsThe average follow-up period of patients was 73.5 months (range, 0-196 months). During the follow-up period, there were 72 cases of recurrence, including 47 cases of loco-regional recurrence and 25 cases of distant metastasis. Additionally, 95 patients died. The 5-year recurrence-free survival rates were 67.2% for the stage I-II group and 64.9% for the stage III-IV group, while the 5-year disease-specific survival rates were 78.2% and 54.5%, respectively (Fig. 1).
In univariate analysis, significant factors associated with disease recurrence were patient age and N classification. In multivariate analysis, considering variables with a p-value ≤0.3, only age and N classification remained significantly correlated with disease recurrence. Based on univariate analysis, significant factors associated with patient mortality included surgical margin, N classification, and NAC. In multivariate analysis, only N classification showed a significant association with patient death (Table 2).
A total of 72 cases of relapse occurred during the research period. Of these, 65.3% experienced loco-regional recurrence, and the remaining 34.7% had distant metastasis. Regional recurrence accounted for 44.4% of all recurrences. The 5-year survival rate for patients with recurrence was 26.2%. Predictive factors for successful salvage treatment were analyzed. Patient age, sex, PNI, ENE, initial tumor stage, and early recurrence (within 6 months) significantly correlated with successful salvage treatment. In multivariate analysis, the patient sex, surgical treatment, and early recurrence were significant predictors of successful salvage treatment (Table 3). Patients who received surgical salvage treatment achieved a 50.0% success rate, while those who received nonsurgical salvage treatment had an 18.1% success rate. The success rate for patients who relapsed within 6 months after initial treatment was 16.1%, whereas patients who relapsed after 6 months had a success rate of 36.5% (Fig. 2).
Comparison of conventional and transoral surgeryAmong the subjects, 118 patients underwent conventional pharyngo-laryngectomy, while 88 patients underwent transoral surgery, which included transoral surgery±NAC. In the conventional pharyngo-laryngectomy group, only 9 (7.6%) patients had NAC, while in the transoral surgery group, 56 (63.6%) patients had NAC. In comparisons between conventional pharyngo-laryngectomy and transoral surgery, significant differences were observed in the history of alcohol use, surgical margins, LVI, PNI, and clinical T classification. Other information is summarized in Table 1.
Disease recurrence occurred in 26 and 46 patients in the two groups, respectively. At the final visit, we checked whether patients were tracheotomized status and survived with functional larynx. In the open treatment group, 42 patients underwent laryngeal preservation at the time of surgery, and 24 patients survived with a preserved functional larynx. All 88 patients who underwent TORS preserved the larynx at the initial surgery, and 41 patients among them survived with a functional larynx at the last visit. No significant difference was observed between the two groups in the proportion of distant metastasis among the number of recurrences.
To compare the treatment results of the two groups, PSM analysis was performed to match patient age, sex, and tumor stage. The results of the matching were summarized in Fig. 3, showing that the propensity scores became more similar and the effect sizes approached zero, indicating successful matching. There was no significant difference in the distribution of T classification between the two groups (Table 4). Since fewer patients underwent transoral surgery±NAC than those who did not, a 1:2 matching was performed. Subsequently, the loco-regional control rate and disease-control rate were compared, with no significant difference noted in the treatment outcomes in the two groups (Fig. 4).
Second primary malignancyDuring the follow-up period, 38 HPSCC patients developed second primary malignancies in the head and neck. These included esophageal cancer in 22 cases, laryngeal cancer in 8 cases, oropharyngeal cancer in 5 cases, hypopharyngeal cancer in 1 case, nasopharyngeal cancer in 1 case, and oral cancer in 1 case. To analyze the treatment results of patients with and without a second primary tumor, we used PSM analysis to match patient age, sex, and tumor stage. Due to the limited number of patients with a second primary tumor, we performed 1:3 matching, and no significant difference was observed between the two groups in 5-year recurrence-free survival and disease-specific survival (Fig. 5).
DiscussionAll HPSCC patients in this study underwent curative surgery and received adjuvant treatment (radiotherapy or CCRT) based on pathological findings. The lack of a statistical difference in recurrence-free survival between the two groups (stage I-II vs. stage III-IV) can be attributed to several factors. Firstly, even early-stage HPSCC patients (stage I-II) had a relatively low recurrence-free survival rate of only 67%, likely due to the high aggressiveness of HPSCC itself. Additionally, the significant difference in the number of patients between the two groups (39 in stage I-II, 169 in stage III-IV) warrants caution when interpreting the survival analysis results. The relatively small number of patients in the early-stage HPSCC group may limit the statistical power for analyzing survival outcomes.
When examining the overall survival plot of HPSCC patients in this study, it’s evident that the survival curve continued to decrease for up to 120 months after the initial treatment. This suggests that factors like medical comorbidities and poor nutritional status, common in HPSCC patients, may have influenced long-term outcomes. As a result, long-term healthcare, regular follow-up, and consultations to monitor general medical health are essential for HPSCC patients. These findings emphasize the need for extended follow-up compared to other head and neck malignancies. In HPSCC patients, age and N classification were identified as prognostic factors for recurrence, while only N classification was associated with survival. Predictive factors for successful salvage treatment included gender, surgical intervention, and early recurrence. Patients who received salvage treatment, including surgery, achieved a 5-year survival rate of 50.0%, whereas patients who did not receive salvage treatment had a lower rate of 18.1%. Notably, for patients who experienced recurrence within 6 months after the initial treatment, the 5-year survival rate was only 16.1%, suggesting a more resistant and aggressive nature of such early recurrent tumors.
The occurrence of secondary primary malignancies is associated with poor prognosis in HPSCC patients. Guo, et al. [12] conducted a surveillance, epidemiology, and end results (SEER)-based study that showed a significantly higher incidence of secondary primary malignancies in HPSCC patients compared to the general population. However, the survival rate of HPSCC patients was not reduced due to the occurrence of secondary primary malignancies. In a study by Yamamoto, et al. [13], secondary primary malignancies were found in 46% of HPSCC patients, with the esophagus being the most common site. The authors emphasized the importance of periodic esophageal surveillance in HPSCC patients. Moreover, it was reported that the survival rate of patients was significantly reduced when secondary primary malignancies occurred synchronously rather than metachronously. In our study, secondary primary cancers developed in 18% of HPSCC patients during the follow-up period, with esophageal malignancy being the most common (n=22). We performed propensity score matching (PSM) for age, sex, and tumor stage to compare treatment outcomes between patients with and without secondary primary malignancies. Statistically, no significant difference was observed in the 5-year recurrence-free survival and disease-specific survival between the two groups, likely because many patients do not survive for a sufficient period due to the aggressive nature of HPSCC.
Classical surgical methods, such as pharyngo-laryngectomy, often necessitate extensive reconstructive surgery and result in high postoperative morbidity. With the advancement of endoscopic instruments and robot technology, research on transoral surgery for HPSCC patients has shown promising treatment outcomes. Transoral surgery combined with NAC has been performed for advanced HPSCC, and favorable oncological and functional outcomes have been reported [8-10]. In our institution, both classical surgery and transoral surgery combined with NAC are used to treat HNSCC patients. Since this study is retrospective, bias in patient selection could not be avoided. To address this, we conducted PSM for comparative analysis of treatment results in the two treatment groups. Due to the relatively small number of patients who underwent transoral surgery combined with NAC, PSM was performed at a 1:2 ratio for patient age, sex, and tumor stage.
When analyzing the loco-regional control rate and disease-control rate in the two groups, no statistically significant differences were observed (Fig. 3). However, in terms of functional outcomes, 40.7% of patients in the pharyngo-laryngectomy group had a functional larynx, while 87.5% of patients in the transoral surgery group retained functional larynx. Regarding oncologic outcomes, both surgical methods showed comparable results, but the transoral surgery group exhibited more favorable outcomes in terms of functionality.
In conclusion, the 5-year survival rate for HPSCC patients who received surgical treatment was 78% for stage I-II and 54% for stage III-IV. While no difference in oncological outcomes was observed based on the surgical modalities, the transoral surgery group showed better functional outcomes. Secondary primary malignancies most frequently occurred in the esophagus, and there was no inferior survival rate in patients with second malignancies.
ACKNOWLEDGMENTSThis work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2021R1C1C1012004).
NotesAuthor contributions Conceptualization: Young Min Park. Data curation: Young Min Park. Formal analysis: Ja Yoon Kim, Young Min Park. Funding acquisition: Young Min Park. Methodology: Young Min Park. Project administration: Young Min Park. Supervision: Young Min Park. Writing—original draft: Ja Yoon Kim. Writing—review & editing: Young Min Park, Jae-Yol Lim, Yoon Woo Koh, Se-Heon Kim. Fig. 1.The differences of 5-year survival rates between the cancer stages. A: The 5-year recurrence-free survival was 67.2% in the stage I–II group and 64.9% in the stage III–IV group. B: The 5-year disease-specific survival was 78.2% in the stage I–II group and 54.5% in the stage III–IV group. 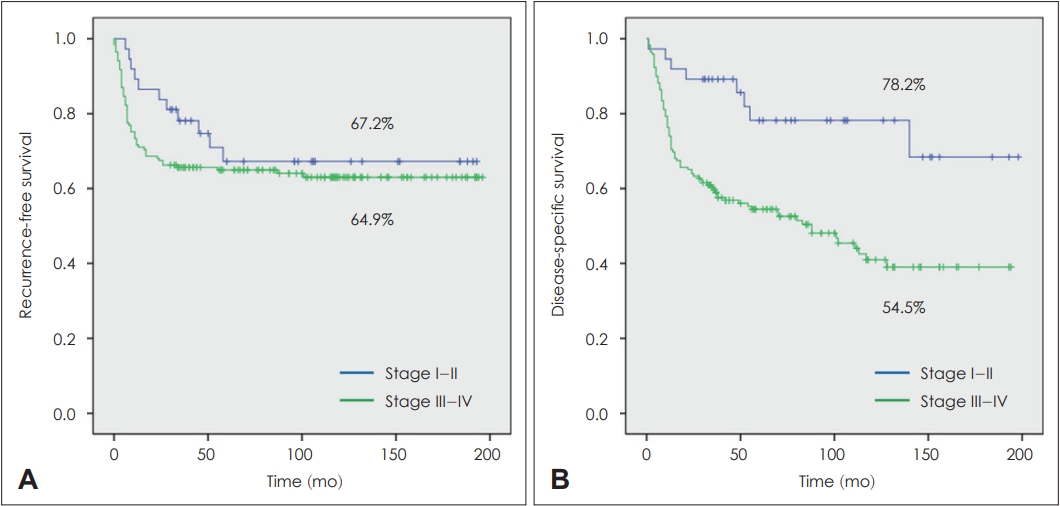
Fig. 2.Salvage success rate for each treatment group. A: Patients who received surgical salvage treatment had a 50.0% salvage success rate, and subjects who received nonsurgical salvage treatment had a salvage success rate of 18.1%. B: The salvage treatment success rate for patients who relapsed within 6 months after initial treatment was 16.1%, and the salvage treatment success rate for patients who relapsed after 6 months was 36.5%. 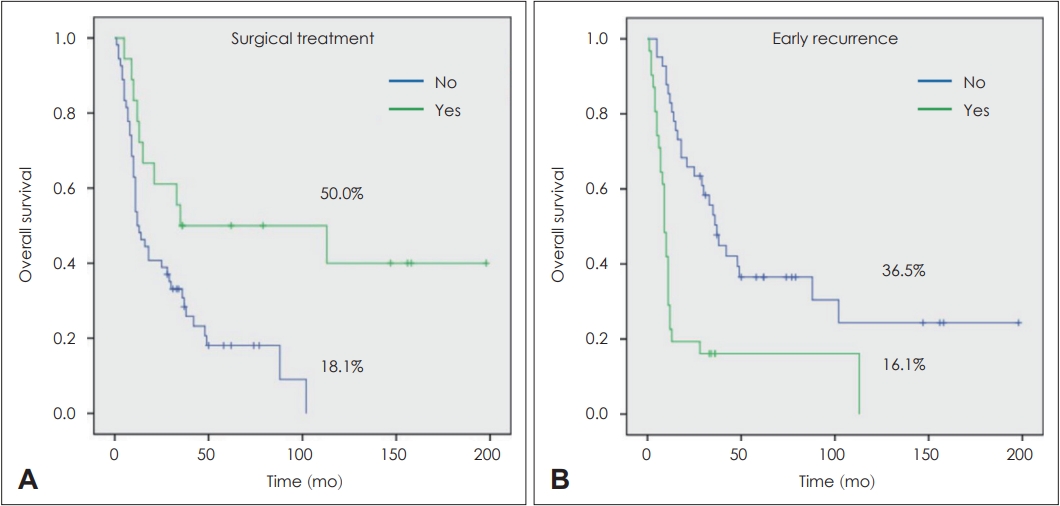
Fig. 3.Propensity score matching (PSM) results. A: Distribution of co-variate before and after matching. B: Effect size of co-variate on PSM analysis. 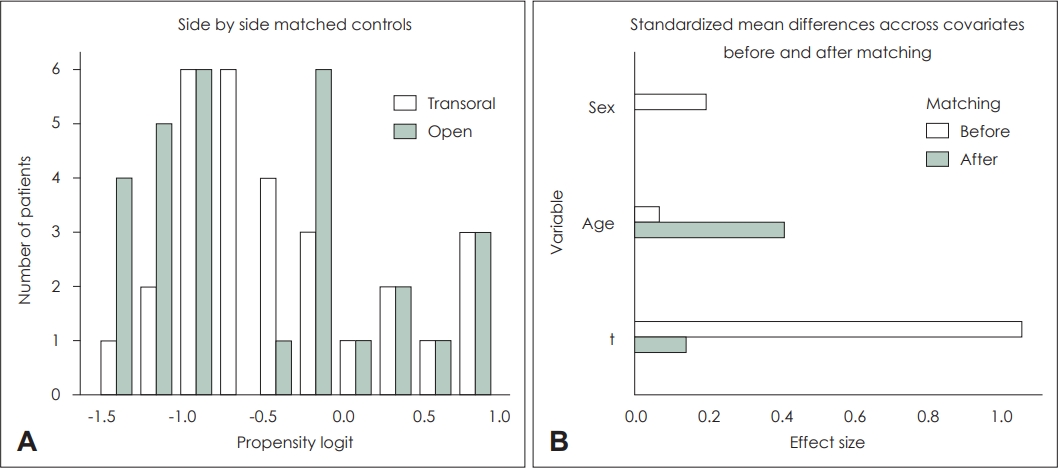
Fig. 4.Loco-regional control rate (A) and disease-control rate (B) were compared and analyzed; significant difference was not observed in the treatment outcomes in the two groups (conventional pharyngo-laryngectomy vs. transoral surgery). OPEN, refers to conventional pharyngo-laryngectomy; TORS, transoral robotic surgery. 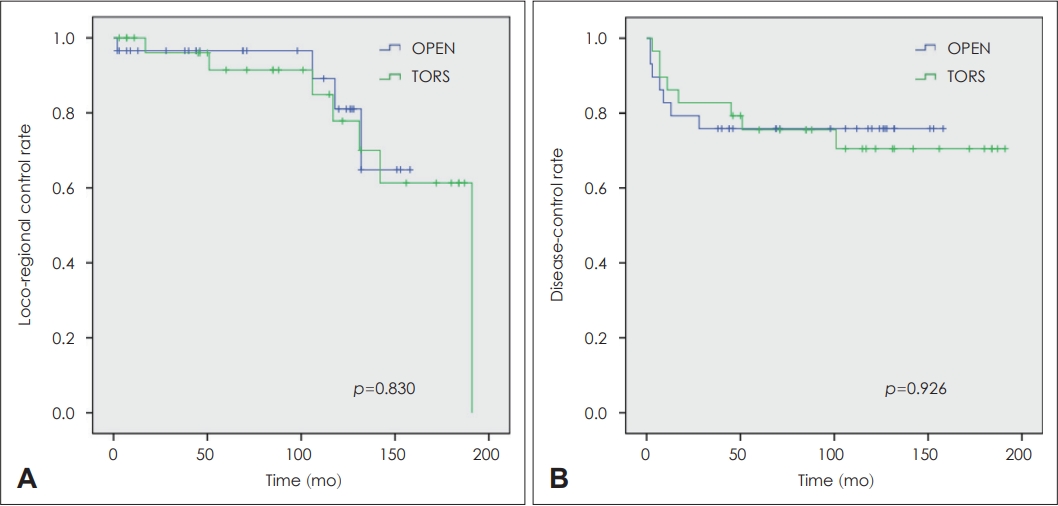
Fig. 5.Significant difference was not observed between the two groups (patients with second primary tumor vs. patients without second primary tumor) in 5-year recurrence-free survival (A) and disease-specific survival (B). 
Table 1.Clinical informations and differences of data between two surgical treatments (conventional pharyngo-laryngectomy vs. transoral surgery) Table 2.Multivariate Cox regression analysis for recurrence-free and disease-specific survival on various factors Table 3.Predicting factors for successful salvage therapy in recurrent cases REFERENCES1. Habib A. Management of advanced hypopharyngeal carcinoma: Systematic review of survival following surgical and non-surgical treatments. J Laryngol Otol 2018;132(5):385-400.
2. Hung LT, Huang HI, Wang LW, Yang MH, Chu PY. Oncologic results and quality of life in patients with squamous cell carcinoma of hypopharynx after transoral laser microsurgery. Lasers Surg Med 2018;50(2):117-24.
3. Kim SY, Rho YS, Choi EC, Kim MS, Woo JH, Lee DH, et al. Clinicopathological factors influencing the outcomes of surgical treatment in patients with T4a hypopharyngeal cancer. BMC Cancer 2017;17(1):904.
4. Lim SH, Lee SJ, Ahn MJ, Park K, Sun JM. Different clinical outcomes between locally advanced hypopharyngeal and oropharyngeal cancer treated with definitive concurrent chemoradiotherapy: Implication for subgroup selection for induction chemotherapy. Jpn J Clin Oncol 2016;46(1):40-5.
5. Joo YH, Cho KJ, Park JO, Nam IC, Kim MS. Role of larynx-preserving partial hypopharyngectomy with and without postoperative radiotherapy for squamous cell carcinoma of the hypopharynx. Oral Oncol 2012;48(2):168-72.
6. Bhayani MK, Hutcheson KA, Barringer DA, Roberts DB, Lewin JS, Lai SY. Gastrostomy tube placement in patients with hypopharyngeal cancer treated with radiotherapy or chemoradiotherapy: Factors affecting placement and dependence. Head Neck 2013;35(11):1641-6.
7. Chen AM, Hsu S, Meshman J, Chin R, Beron P, Abemayor E, et al. Effect of daily fraction size on laryngoesophageal dysfunction after chemoradiation for squamous cell carcinomas of the larynx and hypopharynx. Head Neck 2017;39(7):1322-6.
8. Solimeno LS, Park YM, Lim JY, Koh YW, Kim SH. Treatment outcomes of neoadjuvant chemotherapy and transoral robotic surgery in locoregionally advanced laryngopharyngeal carcinoma. Head Neck 2021;43(11):3429-36.
9. Park YM, Keum KC, Kim HR, Cho BC, Kim DH, Cho NH, et al. A clinical trial of combination neoadjuvant chemotherapy and transoral robotic surgery in patients with T3 and T4 laryngo-hypopharyngeal cancer. Ann Surg Oncol 2018;25(4):864-71.
10. Park YM, Kim DH, Kang MS, Lim JY, Koh YW, Kim SH. Transoral robotic surgery in patients with stage III/IV hypopharyngeal squamous cell carcinoma: Treatment outcome and prognostic factor. Acta Otolaryngol 2019;139(9):816-22.
11. Hall SF, Groome PA, Irish J, O’Sullivan B. The natural history of patients with squamous cell carcinoma of the hypopharynx. Laryngoscope 2008;118(8):1362-71.
|
|
||||||||||||||||||||||||||||||||||||||||||||

 |
 |