 |
 |
AbstractBackground and ObjectivesMaxillary sinus is easily accessible through endoscopic surgery; however, additional combined approaches may be required depending on primary lesions. These approaches are canine fossa approach (CFA), Caldwell-Luc operation (C-L op), Denker approach, and inferior turbinate (IT) swing technique. Our purpose was to analyze and compare the overall results of these surgical approaches to determine superiority.
Subjects and MethodRecords of patients who underwent surgery of functional endoscopic sinus surgery (FESS) with CFA, C-L op, Denker approaches or IT swing technique in a single tertiary hospital from 2015 to 2023 were studied retrospectively. Patients who underwent additional surgery other than CFA, C-L op, Denker, and IT swing technique were excluded.
ResultsA total 86 patients underwent FESS with combined approaches. IT swing technique was used for 30 patients, Denker op was performed for three patients, and C-L op or CFA was used for 53 patients. IT swing technique, Denker op, and C-L op were mainly used for nasal cavity tumor, such as inverted papilloma (IP). CFA was used for not only CRS w NP but also for IP. Recurrence was reported for the IT swing group and CFA group in IP. Three out 20 patients relapsed in the IT swing group, and two out of six patients relapsed in the CFA group.
IntroductionIn functional endoscopic sinus surgery (FESS), the most accessible surgical site of sinus is maxilla. However, the size of maxillary sinus varies from person to person, and access to the lesion is difficult depending on the degree of internal septation [1], the location of the lesion, and anatomical deformities [2,3]. To overcome these difficulties, several surgical approaches to the maxillary sinus have been developed and modified. Starting with traditional Caldwell-Luc operation (C-L op) [4], there is a slightly less invasive approach, which is canine fossa approach (CFA). Anterior and medial access of the maxillary sinus became possible through the Denker op using drill or osteotome [5]. Inferior turbinate (IT) swing technique was recently introduced, and it is minimal invasive technique that made possible for visualization of maxillary sinus anteromedial superior wall which is most difficult site to approach [6].
We would like to compare each surgical approaches combined with endoscopic sinus surgery over past 8 years in a single tertiary hospital, focusing on the pros and cons of IT swing technique.
Subjects and MethodsStudy designThis study used single comparison method and retrospective analysis for patients who underwent combined surgery with endoscopic sinus surgery at a single tertiary hospital from January 2015 to September 2023. Of these, additional surgical approach of modified surgical technique was performed when there was difficulty in visualization and complete removal of lesions.
Operation methodCFA4-5 mm trocar and cannula are used to puncture at the intersection point of the mid pupillary line and the horizontal line passing the lower edge of the nasal alar. Through the puncture site, microdebrider can be inserted to remove the lesion while observing the inside of the maxillary sinus with a 70º endoscope [7].
C-L3-4 cm incision from the lateral incisor to the second molar tooth into the gingivobuccal sulcus and dissect to the periosteum. After exposing the anterior wall of the maxillary sinus by retracting the inner and outer sides of the infraorbital nerve using a retractor, Kerrison rongeur is used to opening anterior maxillary sinus [8].
DenkerUsing monopolar electrocautery, make a mucosal cut to the nasal floor, lateral nasal wall, and anterior head of the inferior turbinate and perform subperiosteal dissection. Create a bony window in the anterior maxilla using a high-speed drill or osteotome. In this process, the nasolacrimal duct should be cut sharply and the infraorbital nerve should be operated with care not to damage it [9].
IT swing techniqueGrip the anterior part of the attachment of the inferior turbinate with a straight Kelly (Fig. 1). Cut with a septal scissor at once, leaving a clear-cut margin. The detachment part of the inferior turbinate is posteriorly rotated to the nasopharynx. After removing the medial wall of maxillary sinus, operation is performed with visualization of entire maxillary sinus [6]. It is mainly used as an additional procedure during modified endoscopic medial maxillectomy for the purpose of securing visual field. When the operation is completed, the rotated IT part is returned to its original position, and the incision site is sutured 1-2 times with Vicryl (absorbable). To prevent IT lateralization, nasal packing with absorbable packing material (ex. Curefoam) on inferior meatus for 2-3 weeks.
Outcome measuresThe number of patients, age, gender, biopsy results, previous surgery history, operation time and revision surgery due to recurrence were verified by classifying them into four groups, such as IT swing group, Denker group, C-L group and CFA group. Side effects were classified as during operation and post-operative complication. Postoperative complications were mainly facial numbness, classified as transient facial numbness lasting within 12 months and permanent facial numbness lasting over 12 months. Lastly, only patients operated with inverted papilloma (IP) were selected and classified into groups to compare the recurrence rate.
ResultsTwo surgeons performed endoscopic sinus surgery (ESS) combined with additional approach in 86 patients for maxillary sinus lesions from 2015 to 2023. It was classified into IT swing group, Denker group, C-L group and CFA group. All IT swing group underwent modified endoscopic medial maxillectomy together.
The mean age ranged from 42.9 to 58.2 on average, and there was no significant difference between groups. Previous operative history was 3 in IT swing group, 2 in Denker group, 2 in C-L op group and 9 in CFA group. Total 16 out of 86 had revision surgeries (Table 1).
The Denker group had the longest operation time of 114 minute, followed by the IT swing group. In both groups, operation time was longer than other groups because tumor surgery such as IP was mainly performed.
Bleeding was the most common intraoperative complication, and there were no cases serious enough to require transfusion or emergency embolization.
The postoperative complications included facial numbness, epiphora and facial pain. In IT swing group, 2 cases had short term facial numbness lasted for 10 days after surgery, and 3 cases of long-term facial numbness of 12 months or more. In Denker group, NLD obstruction was confirmed in 1 out of 3 patients, and the patient underwent DCR. Two patients had facial numbness for more than 12 months in Denker group. Two patients in C-L op group and 1 patient in CFA group had facial numbness lasted more than 12 months.
IT swing was mainly used for IP of maxillary sinus. Total 20 out of 30 patients underwent IT swing combined with MEMM for IP. Other cases were CRS, odontogenic cysts, organizing hematomas and antrochoanal polyps. Denker group had 3 patients of IP. In C-L group, surgery was performed evenly for IP, CRS w NP and benign lesions. CFA was mainly used for CRS w NP and benign lesions such as antrochoanal polyp, allergic fungal sinusitis and fungal ball, but also for IP (Table 1).
In case of recurrence, 3 cases in the IT swing group and 3 cases in the CFA group had relapsed. In IT swing group, all cases were IP. In CFA group, 2 cases were IP and the other case was CRS w NP.
DiscussionWith the rapid development of ESS, surgery for benign sinonasal tumor and malignancy are also actively in progress. Among them, endoscopic resection of IP was first introduced by Waitz in 1992 [10].
In case of IP, it is also called “attachment-oriented surgery” in the sense that it is very important completely remove the origin of the tumor [11]. In order to reduce the recurrence rate, it is necessary to identify the tumor origin and drill the underlying bone along with subperiosteal resection of the area where the tumor was attached [12].
We firstly performed CFA for IP and among them, 2 out of 6 cases had relapsed. As the limitations of CFA, it was confirmed that it was not easy to check tumor origin site through the puncture site if the origin site of the tumor is anterior wall of maxillary sinus, which is a limitation of CFA (Table 2).
In particular, when the tumor origin is attached to the anteromedial side, it was obvious that the operation field or drilling did not proceed sufficiently. Afterwards, in order to secure the field of view of anteromedial side of maxilla, we tried to reduce relapsing cases through performing IT swing technique combined with modified endoscopic medial maxillectomy (MEMM) (Table 2).
Nevertheless, relapsed IP cases were observed in the IT swing group, with 2 cases of tumor originated from the anteromedial superior region (Fig. 2A and D, B and E) and the remaining 1 case from the anteroinferior region (Fig. 2C and F).
Significance of IT swingIn general, inferior turbinate was sacrificed during medial maxillectomy. As a result, crust formation or nasal obstruction could be occurred after medial maxillectomy. Therefore, medial maxillectomy with preserving inferior turbinate has been attempted before and exists in various forms [13]. We preferred surgery with sufficient visualization of maxillary sinus after detachment of IT, and then reconstruct with IT attachment, which was named as IT swing approach [6]. We have experienced IT swing technique for the past 8 years.
Advantages and indications of IT swingIt is possible to prevent the occurrence of empty nose syndrome and atrophic rhinitis that can occur by performing IT sacrifice [14]. If the nasal cavity is enlarged more than necessary, it rather forms an abnormal airflow of nasal cavity and causes dryness or crusts of the mucous membrane [15]. Also, in case of MEMM, it is considered to be less invasive method than Denker and C-L because it can preserve NLD.
Indications for the use of IT swing technique are available for most maxillary sinus lesions (Fig. 3A). In this study, it was mainly applied to sinonasal tumors, because the other lesions can be handled by classic FESS or CFA.
Limitations of IT swingThree out of 20 cases recurred after IT swing and it is thought to be due to incomplete bone drilling of tumor origin. In recurred 3 cases, of which the tumor origin has an irregular contour on the anteromedial superior side and anteroinferior origin, complete removal was difficult. That is the reason for tumor recurrence. Generally, the angles of the drills that can be used was not variable, therefore in some cases, the drill did not reach the bone to which the tumor was attached.
Overcome the limitationIn order to approach drilling in areas that do not reach the tumor origin, drilling of the anterior wall is necessary (Fig. 3B). After drilling, the angle covered by the anterior wall disappears (Fig. 3C). This technique is very useful to secure the endoscopic field of vision even during outpatient clinic follow up after surgery. Nevertheless, the Denker and C-L op were performed for IP patients who thought that the IT swing technique was insufficient, and no recurrence was confirmed in those groups.
Comparison with prelacrimal approachPrelacrimal recess approach is a procedure that allows access to the maxillary sinus by subperiosteal dissection of lateral nasal wall, performing a vertical osteotomy in the space between pyriform aperture and the axilla of the inferior turbinate, and removing the frontal process bone of maxilla through a high-speed drill or chisel [16]. Prelacrimal recess approach is a procedure that first identifies Hasner’s valve and then removes the medial maxilla anterior to it, making it easy to access lesions anterior to the maxilla [17].
The IT swing approach and the prelacrimal recess approach are both meaningful methods for performing a medial maxillectomy. When performing a medial maxillectomy, it is important to preserve Hasner’s valve. The prelacrimal recess approach involves removing the anterior part of the medial maxilla in front of Hasner’s valve, while the IT swing approach allows for a more extensive medial maxillectomy by removing both the anterior and posterior parts of the medial maxilla near the Hasner’s valve.
Limitation and strength of this studyOne limitation of this study is that 1) there may be selection bias in the patient populations for each approach. Typically, surgical methods like CFA were applied to lesions that seemed easily accessible, but in cases where accessing the maxillary sinus appeared difficult, surgical techniques like IT swing or Denker operation were used. Therefore, comparing recurrence rates between approaches may not be appropriate. 2) There are fundamental limitations to retrospective observational studies. However, since there are currently few papers comparing different approaches for challenging maxillary sinus lesions that are hard to access, our study could potentially serve as a cornerstone in this field.
In conclusion, the IT swing technique can be useful in IP where attachment-oriented surgery is important, but it can be limited in the case of severe maxillary contour. If the angle of the drills on the market becomes more diversified, IT swing technique can be more applied to the remove tumors in difficult-to-access locations such as anteromedial superior portion of maxilla.
ACKNOWLEDGMENTSThis work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (No. HI22C1124).
NotesAuthor contributions Conceptualization: Jong Seung Kim. Data curation: Ji Hoon Koh. Formal analysis: Ji Hoon Koh. Funding acquisition: Jong Seung Kim. Investigation: Ji Hoon Koh. Methodology: Ji Hoon Koh. Project administration: Jong Seung Kim. Resources: Jong Seung Kim. Software: Jong Seung Kim. Supervision: Jong Seung Kim. Validation: Jong Seung Kim. Visualization: Ji Hoon Koh. Writing—original draft: Ji Hoon Koh. Writing—review & editing: Jong Seung Kim. Fig. 1.A diagram of Inferior Turbinate swing approach. A: Grip the anterior part of the attachment of the inferior turbinate with a straight Kelly. B: Cut with a septal scissor at once, leaving a clear-cut margin. C: The detachment part of the inferior turbinate is posteriorly rotated to the nasopharynx. D: Medial maxillectomy can be easily done because of rotated inferior turbinate. E: In case of inverted papilloma originated from maxilla anterior wall, sufficient visualization of the anterior wall of the maxilla and drilling of the origin site is necessary. F: The rotated inferior turbinate part is returned and sutured with absorbable suture, when the operation is completed. 
Fig. 2.Representative images of three patients with difficult-to-access origin sites. Axial (A) and coronal (D) T1-weighted gadolinium-enhanced image showing contrast enhancement of inverted papilloma. Tumor originated from anteromedial superior portion of the maxillary sinus. Axial (B) and coronal (E) planes of CT demonstrating heterogenous contrast enhancement by the IP. Tumor originated from anteromedial superior portion of the maxillary sinus. Axial (C) planes of CT demonstrating heterogenous contrast enhancement by the relapsed IP. Axial (F) T1-weighted gadolinium-enhanced image showing contrast enhancement of relapsed IP. Tumor originated from inferomedial portion of the maxillary sinus. 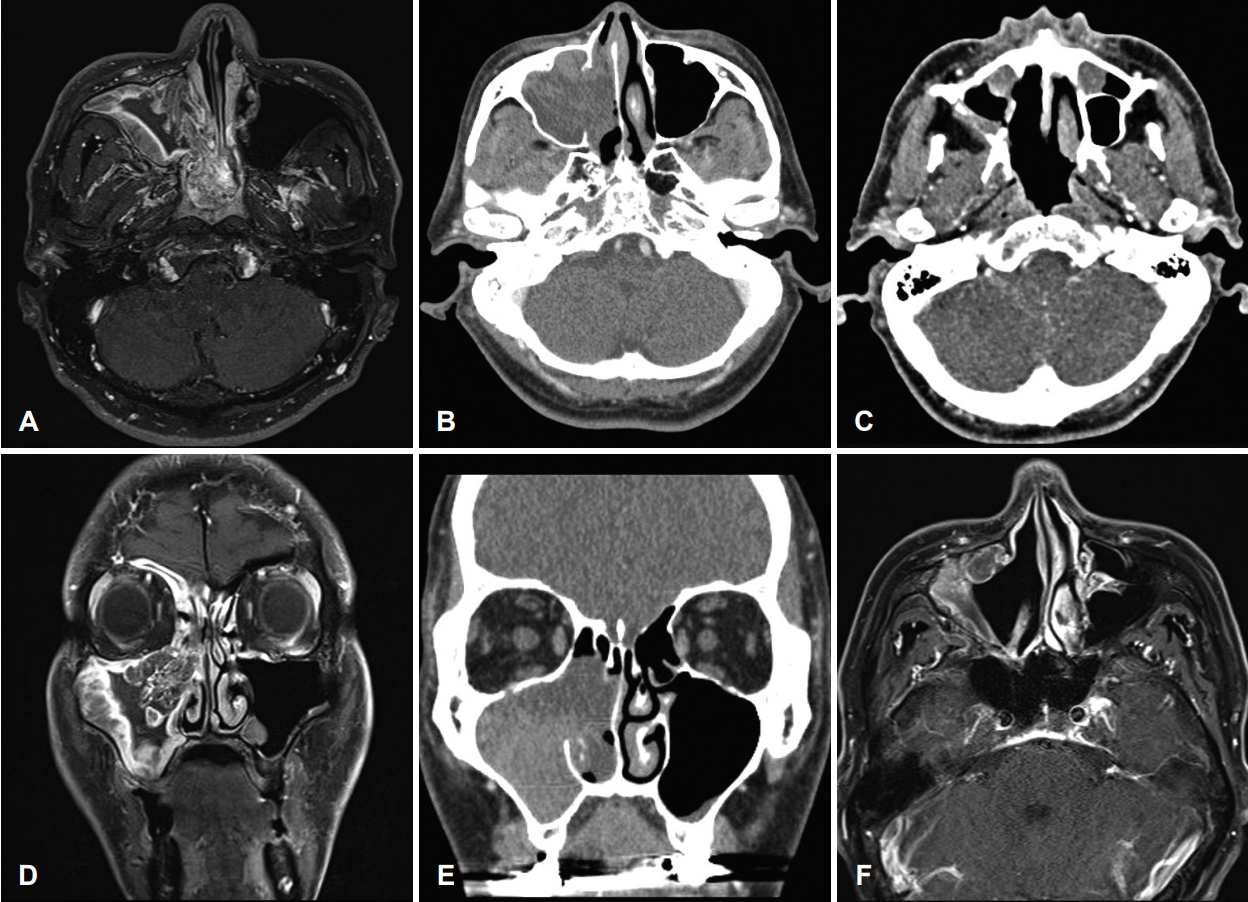
Fig. 3.Schematic diagram of IT swing approach surgery for a maxillary tumor with an anterior wall origin site. A: Inferior turbinate swing technique is available for most maxillary sinus lesions, especially the tumor originating from anterior wall. B: In order to approach drilling in areas that do not reach the tumor origin, drilling of the anterior wall is necessary. C: After drilling, the angle covered by the anterior wall disappears. 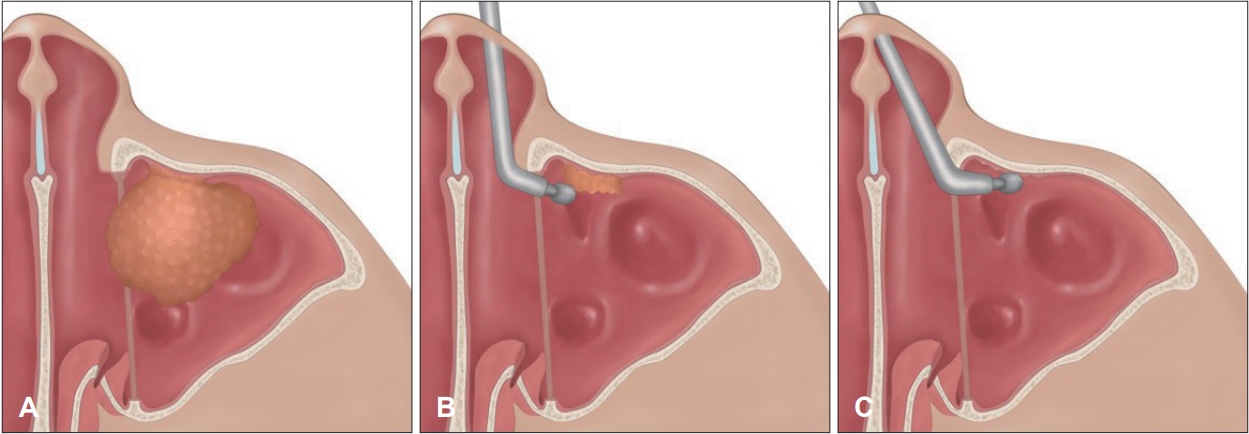
Table 1.General considerations for each group (n=86)
* benign tumor: odontogenic cyst (4; IT swing, 1; C-L), CRS (1; IT swing, 2; CFA), antrochoanal polyp (1; IT swing, 2; C-L, 12; CFA), organizing hematoma (3; IT swing, 2; C-L), allergic fungal sinusitis (1; CFA), fungal ball (1; CFA). IT, inferior turbinate; C-L, Caldwell-Luc operation; CFA, canine fossa approach; Previous op hx, history of previous operations; Op time, operation time (min); Cx, complications; IP, inverted papilloma; CRS, chronic rhinosinusitis; CRS w NP, chronic rhinosinusitis with nasal polyps; Mean f/u, mean follow-up period (months) Table 2.Inverted papillomas REFERENCES1. Rancitelli D, Borgonovo AE, Cicciù M, Re D, Rizza F, Frigo AC, et al. Maxillary sinus septa and anatomic correlation with the schneiderian membrane. J Craniofac Surg 2015;26(4):1394-8.
2. Kakade AG, Chaudhari NH, Baviskar SM, Bagga RR, Patni ZM. Evaluation of variations of maxillary sinus on computed tomography. MVP J Med Sci 2018;5(2):172-7.
3. Lozano-Carrascal N, Salomó-Coll O, Gehrke SA, Calvo-Guirado JL, Hernández-Alfaro F, Gargallo-Albiol J. Radiological evaluation of maxillary sinus anatomy: A cross-sectional study of 300 patients. Ann Anat 2017;214:1-8.
4. Datta RK, Viswanatha B, Shree Harsha M. Caldwell Luc surgery: Revisited. Indian J Otolaryngol Head Neck Surg 2016;68(1):90-3.
5. Ashman A, Psaltis AJ, Wormald PJ, Tan NC. Extended endoscopic approaches to the maxillary sinus. J Laryngol Otol 2020;134(6):473-80.
6. Jung YG, Park GC. Inferior turbinate swing technique: A novel surgical route to approach maxillary sinus area pathology. Otolaryngol Head Neck Surg 2018;159(4):796-8.
7. Anand V, Santosh S, Aishwarya A. Canine fossa approaches in endoscopic sinus surgery - our experience. Indian J Otolaryngol Head Neck Surg 2008;60(3):214-7.
8. Huang YC, Chen WH. Caldwell-Luc operation without inferior meatal antrostomy: A retrospective study of 50 cases. J Oral Maxillofac Surg 2012;70(9):2080-4.
9. Lee JT, Chiu AG. Endoscopic Denker approach for anterior maxilla tumors. In: Chiu AG, Palmer JN, Adappa ND, eds. Atlas of endoscopic sinus and skull base surgery. 2nd ed. Philadelphia, PA: Elsevier; 2019. p. 183-90.e1.
10. Attlmayr B, Derbyshire SG, Kasbekar AV, Swift AC. Management of inverted papilloma: Review. J Laryngol Otol 2017;131(4):284-9.
11. Pagella F, Pusateri A, Giourgos G, Tinelli C, Matti E. Evolution in the treatment of sinonasal inverted papilloma: Pedicle-oriented endoscopic surgery. Am J Rhinol Allergy 2014;28(1):75-81.
12. Landsberg R, Cavel O, Segev Y, Khafif A, Fliss DM. Attachment-oriented endoscopic surgical strategy for sinonasal inverted papilloma. Am J Rhinol 2008;22(6):629-34.
13. Nakayama T, Asaka D, Okushi T, Yoshikawa M, Moriyama H, Otori N. Endoscopic medial maxillectomy with preservation of inferior turbinate and nasolacrimal duct. Am J Rhinol Allergy 2012;26(5):405-8.
14. Coste A, Dessi P, Serrano E. Empty nose syndrome. Eur Ann Otorhinolaryngol Head Neck Dis 2012;129(2):93-7.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |