덱사메타손을 병용한 화학적 미로 절제술에서의 청력 보존 효과
Effect of Dexamethasone Combination With Gentamicin in Chemical Labyrinthectomy on Hearing Preservation in Patients With Meniere’s Disease
Article information
Trans Abstract
Chemical labyrinthectomy may be performed in patients with Meniere’s disease who have intractable vertigo that does not respond to drug. By using aminoglycosides, the surgical procedure ablates vestibular type 1 hair cells. However, the risk of hearing loss remains a main concern for clinicians because gentamicin ablates cochlear hair cells as well as vestibular hair cells. To deal with the concern for hearing loss, dexamethasone can be combined with gentamicin during chemical labyrinthectomy. Herein, we show that chemical labyrinthectomy using gentamicin combined with dexamethasone preserve hearing at high-frequency compared to the conventional method.
Introduction
The clinical feature of Meniere’s disease includes fluctuating sensorineural hearing loss accompanied by aural pressure, tinnitus, and episodic vertigo. As an acute treatment for vertigo attacks, medical treatment such as antihistamine or anticholinergics is used. In contrast, chronic treatment for Meniere’s disease aims to reduce the frequency of vertigo attacks and prevent aggravation of ear symptoms. It starts with lifestyle modification such as reducing salt intake, avoiding caffeine and medical treatment including diuretics. If there is no response to drug, intratympanic corticosteroid (ITC) injection is generally considered as second-line treatment [1]. However, patients irresponsive to second-line treatment require tertiary treatment which commonly involves surgical intervention.
Chemical labyrinthectomy is a surgical procedure which ablates vestibular type 1 hair cells using aminoglycosides [2]. Direct application of gentamicin to the middle ear through explotympanotomy guarantees the accurate and sustained application of the drug compared to intratympanic injection of the solution. However, in both methods, the risk of hearing loss by gentamicin remains a main concern for clinicians because gentamicin ablates cochlear hair cells as well as vestibular hair cells. Half the patients treated with repetitive systemic high-dose aminoglycoside therapy suffered hearing loss at high-frequency level [3]. Hearing level can decline up to 31.08% after chemical labyrinthectomy with gentamicin depending on the administration and titration method [4,5].
Corticosteroid, including dexamethasone, can be used in sudden onset hearing loss or vertigo in various method of administration [6,7]. The effect of intratympanic dexamethasone injection in controlling Meniere’s disease is also previously reported [8]. To deal with the concern for hearing loss when using gentamicin, the dexamethasone can be combined with gentamicin during chemical labyrinthectomy [9]. The result of the combination method is promising in the preservation of highfrequency hearing although a small number of patients were enrolled.
Methods
Patient enrollment
From 11 November 2015 to 15 July 2020, total 37 patients diagnosed for definite Meniere disease (MD) with intractable vertigo attacks received chemical labyrinthectomy. This study was approved by the Institutional Review Board of Severance Hospital (Seoul, Korea) before patient enrollment (Project number 4-2016-0096). Written informed consent was provided to every participants. The inclusion criteria were 19 years or older patients who were diagnosed with definite MD and had intractable vertigo attacks although medication and lifestyle modification. The patients with a history of head trauma, central vertigo, another otologic disease, or suspected bilateral MD were excluded from the study.
Patients with intractable vertigo were treated with betahistidine and diuretics, along with lifestyle modifications for more than three months, and intratympanic dexamethasone injection was performed since medication and lifestyle modification showed no improvement. Nonetheless, the number of vertigo attacks was not decreased in the following three months after ITC injection. The vertigo attack was defined as more than 20 minutes of spontaneous true-vertigo regardless of ear symptoms. A total of 18 patients conducted dexamethasonecombination (GD group) chemical labyrinthectomy after randomization. Other 19 patients conducted saline-combination (GO group) chemical labyrinthectomy.
Chemical labyrinthectomy procedures
After local anesthesia at external auditory canal, tympanomeatal flap was elevated to expose the oval window and round window. And then, gentamicin-soaked Gelfoam® (Pfizer, New York, NY, USA) was applied to the oval window, and according to the patient group, saline-soaked Gelfoam® or dexamethasone-soaked Gelfoam® was applied to the round window (Fig. 1). A sufficient volume of Gelfoam® should be applied to achieve the appropriate effect of drug administration. Using extremely small pieces of Gelfoam® is recommended to prevent dead space in the round window niche. Meticulous bleeding control should be performed to prevent the mixing of two different drugs. Then, reposit tympanomeatal flap and apply Gelfoam® on the incision site (Supplementary Video 1).

Endoscopic chemical labyrinthectomy was performed to a 53 years old female suffering from unilateral Meniere disease. (A) In the middle ear cavity, oval window and round window could be found (B) gentamicin-soaked Gelfoam® (Pfizer) was applied to oval window (C) dexamethasone-soaked Gelfoam® was applied to round window. Red arrow indicates oval window covered by stapes foot plate. Black arrow indicates round window niche.
Results
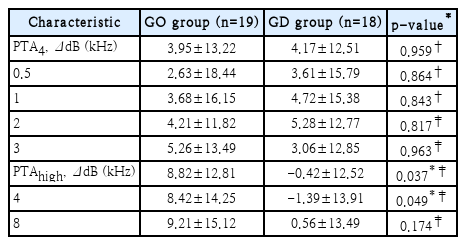
The hearing function was evaluated by pure tone audiometry (PTA) before the chemical labyrinthectomy and 2 months after the procedure. PTA thresholds were compared before and after surgery within each group. In GO group, PTA threshold in 4 kHz (p=0.005) and 8 kHz (p=0.012) frequencies were significantly increased after the chemical labyrinthectomy compared to PTA threshold before the procedure. However, in GD group, PTA threshold were not significantly changed in all frequencies, including in 4 kHz and 8 kHz (Fig. 2). In addition, it was compared whether there was a significant difference in the changed values of the PTA threshold for each frequency between the two groups. There is a significant difference (p=0.037) in PTAhigh, especially in 4 kHz frequency threshold (p=0.049). Other parameters were not significantly different between two groups (Table 1).
Hearing functions before and after chemical labyrinthectomy. A: Pure-tone audiogram of GD group. B: Pure-tone audiogram of GO group. The high-frequency hearing thresholds (4 and 8 kHz) significantly worsened eight weeks after chemical labyrinthectomy only in the GO group. The black/hollow circles indicate median values. The error bars indicate the interquartile range. Wilcoxon matched-pairs signed rank test was used for analysis. *p<0.05; †p<0.01. GD, gentamicin combined with dexamethasone; GO, gentamicin combined with normal saline; Pre, before surgery; Post, eight weeks after surgery.
Chemical labyrinthectomy using gentamicin combined with dexamethasone relatively preserved hearing at high frequency compared to the conventional method using gentamicin and normal saline. Vestibule is adjacent to oval window whereas scala tympani has no communication to the vestibular organ. Therefore, gentamicin applied on the oval window, as in this study, diffuses to the vestibule easily while dexamethasone applied on the round window diffuses to the cochlea more easily due to the anatomical structure [10].
Since both windows are located at the basal turn of the cochlea, the drug concentration would display a gradient from base to apex of cochlea, which corresponds to the tonotopical map of high to low frequency. High-frequency hearing is predicted to be more sensitive to drug administration for this reason [11]. As explained above, it is well known that steroids are effective in preventing hearing deterioration and controlling vertigo. Therefore, by applying dexamethasone to the basal turn of cochlear, it could be possible to prevent hearing loss at high-frequency according to the results of our study. Although the low-frequency hearing may also have been preserved by dexamethasone, it could have been hidden due to the low-frequency fluctuation, the feature of meniere’s disease.
Dexamethasone has been reported to have protective effect on gentamicin induced ototoxicity [12]. Despite the enigma of the exact mechanism of gentamicin-induced hair cell damage remains unsolved, the cell apoptosis pathway via reactive oxygen species formation is suggested to play a main role.
In conclusion, the direct administration of gentamicin combined with dexamethasone to the middle ear can preserve high-frequency hearing.
Supplementary Material
The Data Supplement is available with this article at https://doi.org/10.3342/kjorl-hns.2022.00563.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (NRF-2022R1A2C1008636).
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Severance hospital (Project number 4-2016-0096 and date of approval)
Notes
Author Contribution
Conceptualization: Sung Huhn Kim, Jeon Mi Lee. Formal analysis: Seong Hoon Bae, Hyun Jin Lee, Jeon Mi Lee. Investigation: Seong Hoon Bae, Hyun Jin Lee, Gina Na, Jeon Mi Lee. Supervision: Sung Huhn Kim. Writing—original draft: Yujin Lee, Seong Hoon Bae. Writing—review & editing: Yujin Lee, Seong Hoon Bae, Sung Huhn Kim.