비대칭성 난청 및 일측 전농 환자에서 Bonebridge 이식의 이명에 대한 효과
Effect of Bonebridge Implantation on Tinnitus in Patients With Asymmetric Hearing Loss or Single-Sided Deafness
Article information
Trans Abstract
Background and Objectives
The objective of this study was to investigate the effect of an active transcutaneous bone conduction implant (BCI) of Bonebridge (MED-EL) on tinnitus patients with asymmetric hearing loss (AHL) or single-sided deafness (SSD).
Subjects and Method
Medical records and tinnitus questionnaires were reviewed retrospectively of patients with AHL or SSD, who received Bonebridge by a single surgeon at Seoul St. Mary’s Hospital from 2017 to 2021. Audiologic evaluation and tinnitus questionnaires were conducted before and after surgery.
Results
Of the 17 patients, 8 patients had SSD and 9 patients had AHL, and 13 patients (76.47%) had tinnitus before surgery while 4 patients did not. No patient showed newly developed tinnitus after surgery. After implantation, three patients (23.08%) showed a complete resolution of tinnitus. All patients showed significant improvement in hearing level after surgery. The mean tinnitus handicap inventory (THI) score and visual analogue scale (VAS) score for effect on life showed a significant decrease after surgery, from 43.1±28.2 to 29.7±25.7 (p<0.05), and 4.7±2.9 to 3.2±3.3 (p<0.05), respectively. The mean THI scores of seven AHL patients and seven patients with tinnitus on the implanted ear were significantly decreased after implantation from 50.9±24.7 to 34.6±27.5 (p<0.05) and from 53.1±23.4 to 37.4±15.0 (p<0.05), respectively.
Conclusion
BCI seems to be effective in suppressing tinnitus in the patients with AHL but not with SSD. Along with directive counseling, sound therapy with Bonebridge can decrease tinnitus in some patients with AHL.
Introduction
Patients with sensorineural hearing loss (SNHL) frequently experience tinnitus, and many studies have reported that cochlear implants (CI) are effective in suppressing tinnitus [1,2]. Bone conduction implants (BCIs) provide an optimal option for managing patients with single sided deafness (SSD) or asymmetric hearing loss (AHL), and current alternatives include CIs, contralateral routing of signals (CROS) hearing aids and bilateral microphones with contralateral routing of signals (Bi-CROS) hearing aids. Active transcutaneous BCIs, such as the Bonebridge (MED-EL, Innsbruck, Austria), actively creates and transmits vibrations directly to the skull, achieving better audiologic gain than skin-drive BCIs [3]. In addition, the bone conduction floating mass transducer (BC-FMT) of the Bonebridge is placed in a subperiosteal plane, thus reducing the rate of post-operative complications such as skin regrowth and infection [4].
Although many studies have reported the beneficial effect of the Bonebridge on hearing [3-7], to the best of our knowledge, there has been only one other study by Lee, et al. [8] regarding the effect of the Bonebridge on tinnitus. Thus, in this study, we investigated the effect of the Bonebridge on tinnitus as a sound therapeutic modality of tinnitus in patients with AHL or SSD.
Subjects and Methods
Medical records of patients were reviewed retrospectively. Patients with AHL or SSD who received unilateral Bonebridge (MED-EL) implantation by a single surgeon (S.N.P.) at Seoul St. Mary’s Hospital from 2017 to 2021 were included in this study. We defined AHL as air conduction thresholds ≥60 dB HL in the affected ear and ≤30 dB HL in the unaffected ear and SSD as air conduction thresholds ≥90 dB HL in the affected ear and ≤30 dB HL in the unaffected ear. Exclusion criteria were 1) patients with current external, middle or inner ear deformity and 2) patients with incomplete tinnitus questionnaires.
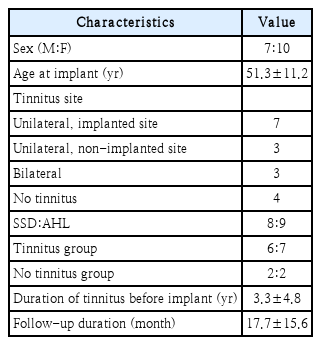
A total of 17 patients were included in this study; 8 patients had SSD, and 9 patients had AHL. Audiologic evaluation and tinnitus questionnaires were conducted before and after surgery. Audiologic evaluation was performed with pure tone audiometry (PTA) and speech discrimination score (SDS), and average air conduction hearing levels of 0.5, 1, 2, and 4 kHz were recorded. Patients with tinnitus received directive counseling of tinnitus rehabilitation therapy by a specialist in the tinnitus clinic. Tinnitus questionnaires comprising of tinnitus handicap inventory (THI) score, awareness of tinnitus and visual analog scale (VAS) score for loudness, annoyance and effect on life were administered.
SPSS software (ver. 24.0; IBM Corp., Armonk, NY, USA) was used for statistical analysis and a p-value<0.05 was considered significant. This study was carried out in accordance with the Declaration of Helsinki on biomedical research for human subjects, and this study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital (KC21RASI0563).
Results
The mean follow-up period of the 17 enrolled patients was 17.7±15.6 months, and the average age at the Bonebridge implantation was 51.3±11.2 years. Of the 17 patients, 8 patients had SSD, and 9 patients had AHL. Thirteen patients (76.47%) had tinnitus before surgery, while 4 patients did not have tinnitus (Table 1). No patient showed newly developed tinnitus after surgery. All patients showed improvement in hearing level after surgery (Table 2). Overall, the average air conduction hearing level of PTA of the implanted ears before surgery was 87.5±21.1 dB and was significantly improved to 34.5±9.1 dB after surgery (p<0.05). The average SDS of the implanted ears was also statistically significantly improved to 46.8%±21.6% after surgery, compared to 10.6%±16.6% before surgery (p<0.05). The average air conduction hearing level of PTA and the average SDS of the non-implanted ears did not show a significant change after surgery.
Of the 13 patients with tinnitus before surgery, 6 patients had SSD, and 7 patients had AHL; 7 patients had unilateral tinnitus on the implanted side, 3 patients had unilateral tinnitus on the non-implanted side, and 3 patients had bilateral tinnitus (Table 1). The mean duration of tinnitus before the Bonebridge implantation was 3.3±4.8 years. Overall, THI score, awareness of tinnitus and VAS score for loudness, annoyance and effect on life were all decreased after surgery, but these changes were only statistically significant in the THI score and VAS score for effect on life, from 43.1±28.2 to 29.7±25.7 (p<0.05), and 4.7±2.9 to 3.2±3.3 (p<0.05), respectively (Table 3 and Fig. 1A). Six SSD patients with tinnitus showed decrease of mean THI score and improvement in mean awareness, VAS score for annoyance and effect on life after implantation, but with no statistical significance. 7 AHL patients with tinnitus showed statistically significantly decrease of mean THI score from 50.9±24.7 to 34.6±27.5 (p<0.05), and improvement in awareness and VAS score for loudness and effect on life after implantation, but with no statistical significance (Table 3 and Fig. 2B).

Pre- and post-operative tinnitus evaluation of the overall patients with tinnitus. A: Tinnitus questionnaire scores of the patients. B: Severity of tinnitus by handicap grade. Wilcoxon signed rank test, *p<0.05. THI, tinnitus handicap inventory; AW, awareness; LD, VAS for loudness; AN, VAS for annoyance; EOL, VAS for effect on life. VAS, visual analogue scale.

Pre- and post-operative tinnitus evaluation of the SSD and AHL patients with tinnitus. A: SSD patients with tinnitus. B: AHL patients with tinnitus. Wilcoxon signed rank test, *p<0.05. THI, tinnitus handicap inventory; AW, awareness; LD, VAS for loudness; AN, VAS for annoyance; EOL, VAS for effect on life. SSD, single-sided deafness; AHL, asymmetric hearing loss; VAS, visual analogue scale.
Of the 17 patients, 13 patients had tinnitus before surgery; 7 patients had tinnitus on the implanted side, 3 patients had tinnitus on the non-implanted side, and 3 patients had bilateral tinnitus (Table 1). Seven patients with tinnitus on the implanted side showed statistically significant decrease of mean THI score after the Bonebridge implantation from 53.1±23.4 to 37.4±15.0 (p<0.05). Mean awareness and VAS scores for annoyance were decreased from 82.9±28.7 to 62.9±39.9 (p=0.115) and 5.4±2.8 to 4.1±2.4 (p=0.671), respectively, but did not show statistical significance. Three patients with unilateral tinnitus on the non-implanted side showed a decrease of mean THI score after the Bonebridge implantation from 39.4±19.0 to 22.2±19.8 (p=0.225). Mean Awareness (%) and VAS scores for loudness, annoyance, and effect on life were all decreased from 39.8±18.7 to 31.1±30.9 (p=0.500), 4.5±2.1 to 2.6±2.2 (p=0.138), and 3.9±1.9 to 3.0±2.5 (p=0.500), respectively. All 3 patients with bilateral tinnitus showed improvement in tinnitus on both sides. Mean THI score was decreased from 44.0±40.2 to 38.7±43.9 (p=0.102). Mean Awareness (%) and VAS scores for annoyance, and effect on life were all decreased from 100.0±0 to 73.3±46.2 (p=0.317), 5.3±1.5 to 3.7±3.2 (p=0.180), and 5.3±3.1 to 5.0±3.6 (p=0.317), respectively.
The severity of tinnitus of the 13 patients with tinnitus before surgery was graded according to the five-point grading scheme proposed by McCombe, et al. [9]: slight (THI 0-16), mild (THI 18-36), moderate (THI 38-56), severe (THI 58-76), and catastrophic (THI 78-100). Of these 13 patients, 9 patients showed moderate, severe or catastrophic handicap before surgery. After surgery, the number of patients with moderate, severe or catastrophic handicap was decreased to 6 patients, showing a 30% reduction. Five patients (38.46%) showed improvement, 8 patients (61.54%) showed no change, and no patient showed exacerbation in the grading of tinnitus severity (Fig. 1B).
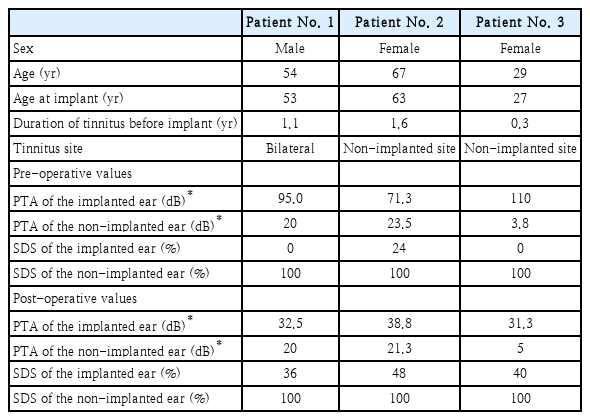
Interestingly, after the Bonebridge implantation, 3 patients (23.1%) showed a complete resolution of tinnitus; the clinical characteristics and pre- and post-operative tinnitus evaluation of these 3 patients are described in Table 4 and Fig. 3, respectively. Two patients had SSD, and 1 patient had AHL. All 3 patients showed a great reduction in all aspects of the tinnitus questionnaire, except for VAS for loudness in Patient No. 1. Additionally, compared to the mean duration of tinnitus before the Bonebridge implantation of 3.3±4.8 years (Table 1), these 3 patients showed relatively shorter duration of tinnitus before implant (Table 4). No patient declined to wear a sound processor of the Bonebridge for any reason.
Discussion
Patients with SSD or AHL have profound hearing loss in the affected ear and nearly normal hearing level in the contralateral ear, resulting in reduced speech perception and impaired sound localization. In addition to impairment in binaural hearing, patients with SSD or AHL often experience concomitant tinnitus which affects their quality of life. CI, CROS or Bi-CROS hearing aids, and BCIs such as the Bonebridge are possible options for treating SSD or AHL. CI restores auditory input to the affected ear by directly stimulating the auditory nerve, while CROS or Bi-CROS hearing aids and BCIs reroute sound from the affected ear to the unaffected ear.
Previous studies have shown that CI is effective in reducing tinnitus in SSD patients [10]. It has been proposed that CI suppresses tinnitus by electrical stimulation of the auditory nerve and cortical reorganization of the auditory pathway [11]. CI restores peripheral auditory input, which act as an inhibiting stimulus to the central nervous system to reduce tinnitus [12].
To the best of our knowledge, only one other study has reported the effect of the Bonebridge in tinnitus to date. Lee, et al. [8] reported in 2020 that the Bonebridge implantation can reduce tinnitus in patients with SNHL. They suggested that masking effect and bidirectionality of the central auditory pathway could explain tinnitus suppression in the Bonebridge recipients. The results from our study support their findings; SSD patients and AHL patients both showed improvement in tinnitus after Bonebridge implantation.
Tinnitus questionnaires conducted by Lee, et al. [8] included THI score, awareness of tinnitus and VAS score for loudness and annoyance; of these questionnaires, THI score, awareness of tinnitus and VAS score for annoyance showed a statistically significant decrease after surgery. In our study, we additionally conducted VAS score for effect on life. Overall, the mean scores of tinnitus questionnaires were all decreased post-operatively; however, only the improvement in the THI score and VAS score for effect on life after surgery were statistically significant. In addition, 3 of 13 (23.1%) patients who had tinnitus before the Bonebridge implantation showed a complete resolution of tinnitus after surgery in our study.
In contrast to CI, BCIs such as the Bonebridge do not directly stimulate the auditory nerve or restore auditory input to the affected ear. Bonebridge reroutes the sound from the affected ear to the unaffected ear, thereby amplifying sound input. All patients in this study showed improvement in hearing after the surgery, and the average PTA and SDS were statistically significantly improved after the implantation. As suggested by Lee, et al. [8], the amplification of the external sound input after the Bonebridge implantation could suppress tinnitus by masking effect.
In this study, 7 patients with tinnitus on the implanted side showed statistically significant improvement of THI score after the Bonebridge implantation. This could be explained by the bidirectionality of the central auditory pathway; auditory information is transmitted from the peripheral to central pathway and crosses at the ipsilateral cochlear nucleus to the contralateral side of the brainstem and brain. Increased sound input in the normal ear after the Bonebridge implantation could be transmitted to the contralateral side of the brainstem and brain, thus suppressing tinnitus on the affected ear. This can be supported by the study that reported contralateral tinnitus suppression after CI [13].
In addition to the masking effect and bidirectionality of the central auditory pathway that Lee, et al. [8] suggested as possible mechanisms for tinnitus suppression in the Bonebridge, alleviation of emotional distress after the Bonebridge implantation could be another possible mechanism of tinnitus suppression. Patients with hearing loss experience emotional distress due to social isolation, which could lead to depression [14]. Jastreboff’s neurophysiological model of tinnitus suggests that activation of limbic and autonomic nervous system in response to emotion can cause tinnitus [15]. Bonebridge implantation does not achieve true binaural hearing, but it improves speech perception and subjectively perceived sound quality of the patients [5]. Improvement of speech perception after implantation allows reduction in emotional distress of the patients, thus possibly reducing tinnitus. In this study, the number of the patients with moderate, severe or catastrophic handicap of tinnitus measured by THI decreased from 9 to 6 after implantation, showing a 30% reduction. Five patients (38.46%) showed improvement in the grading of tinnitus severity, and no patient showed exacerbation. In other words, patients tend to show improvement in the severity of tinnitus and less handicap due to tinnitus after the Bonebridge implantation. Additionally, VAS score for effect on life was statistically significantly improved after surgery, suggesting positive impact on life after surgery. Improvement of tinnitus after surgery in patients with unilateral tinnitus on the non-implanted side and bilateral tinnitus also reinforces this possible mechanism; Bonebridge implantation allows patients with SSD or AHL to hear sounds from the affected ear and enhances speech perception, thus alleviating emotional distress and reducing tinnitus.
In this study, 7 AHL patients with tinnitus showed statistically significant decrease of mean THI score, while 6 SSD patients did not show statistically significant improvement of the aspects of tinnitus questionnaire. Further study needs to be done with a larger sample size to scrutinize on the difference of the effect of BCIs on patients with AHL and patients with SSD.
In summary, improvement of tinnitus after bone bridge implantation in the patients with AHL was observed in this study. We propose several possible mechanisms of the effect of BCI on tinnitus. The sound signal from the deafened or worse hearing side through BCI can modify bidirectionality of the central auditory pathway or may reorganize central pathway of tinnitus in the brain. Decreased stress resulted from better hearing condition after BCI may also affect the central neuronal network of tinnitus, especially in stress related region, to improve tinnitus. In the patients with AHL, enhanced sound and speech signals to the implanted side can also play an important role as a sound therapy.
The limitations of this study include a small sample size and the retrospective study design. In addition, this study design does not include a control group to compare with. A randomized controlled study with a larger sample size is recommended for further studies.
In conclusion, BCI seems to be beneficial in improving hearing level and suppressing tinnitus in the patients with AHL, but not SSD. We propose that possible mechanisms of BCI in reducing tinnitus could be the sound therapeutic effect of masking, bidirectionality of the central auditory pathway, and alleviation of emotional distress.
Acknowledgements
This research was supported by National Research Foundation of Korea (2021R1F1A1049965).
Notes
Author Contribution
Conceptualization: Yeonji Kim. Data curation: Jae Sang Han, Celeste Ann Chua. Funding acquisition: Shi Nae Park. Investigation: Yeonji Kim. Methodology: Yeonji Kim, Jae Sang Han. Supervision: So Young Park, Shi Nae Park. Validation: Jae-Hyun Seo. Visualization: Yeonji Kim. Writing—original draft: Yeonji Kim. Writing—review & editing: Shi Nae Park.