 |
 |
AbstractComplete surgical removal of tumor is a main treatment strategy of auricular squamous cell carcinoma (SCC). However, the appropriate reconstruction of the defect should also be carefully planned because of an aesthetic importance of the auricle. A local flap has a better functional advantage than a free flap for minor defects and therefore it should be primarily considered if possible. With a review of literature, we propose a case of auricular SCC which was successfully treated by wide resection and reconstructed by local rotatory flap.
IntroductionSquamous cell carcinoma (SCC) of external ear accounts for 6%-10% of all malignant skin tumors with predominance in male over 60 years old [1]. Because high rate of local recurrence and lymph node metastasis are reported in SCC of external ear, complete surgical excision with sufficient safety margin is important [1,2]. Moreover, physician should select appropriate reconstruction method of the defect, considering the aesthetical importance of auricle. Herein, the authors report a case of SCC in auricle managed with wide excision and local rotatory flap reconstruction.
CaseA 63-year-old white male in otherwise good health visited our clinic with 1 year history of a growing mass in the right auricle. SCC was confirmed from the punch biopsy preformed 2 weeks ago in another tertiary medical center. The mass was erythematic and about 1×1 cm sized with central ulceration and crust. It was located near cymba concha and antihelical rim of the auricle, with concurrent erythematic swelling of nearby skin (Fig. 1A). There was no gross tumor invasion seen in cartilaginous external auditory canal (EAC). In the temporal bone CT and MRI scan, diffuse swelling of auricle and cartilaginous EAC was seen (Fig. 1B and C). PET scan showed increased uptake (maximum standardized uptake values=17.7) in right auricle. There was mild uptake in right parotid gland, but the fine needle aspiration biopsy result was reactive hyperplasia (Fig. 1D).
We planned wide excision of the tumor and additional sleeve resection if needed. For the reconstruction of auricular defect, we designed local rotatory flap from temporal or buccal area (Fig. 2). After that, we carefully examed a margin of tumor in the operation room by microscope. The tumor seemed to be limited in the auricular portion, not invading inlet of the cartilaginous EAC. There was focal invasion of tumor in the auricular conchal cartilage and the removal of conchal cartilage near invaded area was proceeded. We proceeded wide excision of the tumor including about 1 cm of safety margin around the lesion, including removal of conchal cartilage near the tumor invasion. There was no cancer cell seen in frozen biopsy from resection margin (Fig. 3).
Local rotatory buccal flap was selected for reconstruction. We checked the location of feeding artery by doppler probe and used it for the axis of rotation (Fig. 4A). Then, we elevated the flap over the layer of superficial musculoaponeurotic system, with sufficient amount of subcutaneous tissue (Fig. 4B). The flap was rotated to the auricular defect in a folded shape. The skin fold was made to reconstruct the shape of helix crus and conchal area (Fig. 4C). Donor and receiver site was primarily sutured. EAC opening was reconstructed by fixation of the end of flap into the posterior EAC inlet (Fig. 4D). After the reconstruction, compression dressing was done.
In the pathologic report, the tumor was 1×1.5 cm size and depth of invasion was 4 mm. There was focal involvement of tumor in the conchal cartilage. Partial keratinization pattern was seen and immunohistochemistry stain of cytokeratin AE1/AE3 was positive. Resection margin was clear with 1-1.3 cm of safety margin. There was no lymphovascular invasion. The tumor was finally diagnosed to moderately differentiated SCC (Fig. 5). After the multidisciplinary team approach, the patient was decided to follow up periodically in outpatient clinic for close observation for recurrence, without further adjuvant management. 12 weeks after surgery, the patient is under follow-up in our outpatient clinic without evidence of recurrence (Fig. 6).
DiscussionCurrent treatment of choic in cutaneous SCC is surgical resection of the tumor [3]. Since Frederic Mohs first introduced microscopic controlled method of cancer excision in the 1940s [4], surgical technique called Mohs micrographic surgery (MMS) has been developed until recently [5]. However, because there is no randomized controlled trials or prospective cohort studies comparing MMS with other surgical modality, standard wide excision still remains for a good alternative treatment option [3]. Moreover, in case of SCC invading cartilaginous EAC, sleeve resection is needed for favorable oncological outcome [6].
In this case, it was uncertain whether the cancer invaded EAC because the preoperative imaging (CT, MRI and PET) showed a possibility of EAC involvement. Therefore, the extension of surgery was depended on the intra-operative frozen biopsy result of tumor margins near EAC orifice. Pre-operative preparation of sleeve resection was inevitable for in case the EAC was invaded. Moreover, invasion depth of tumor seemed deep enough to require reconstruction of sufficient volume. In general, there was prominent erythematic swelling in skin around the tumor abutting to helical rim, probably due to inflammatory reaction after punch biopsy which was performed 2 weeks ago. This inflammatory skin change made us even harder to estimate the exact extent of the cancer invasion. In consultation with a plastic surgeon, we decided to prepare local rotatory flap for reconstruction.
Recent study of the auricle SCC proposed the indication of adjuvant radiotherapy in the case of lymphovascular invasion, poorly differentiated type cancer and selected cases with close margins or incomplete excision [7-9]. In this case, the pathologic report showed the absence of lymphovascular invasion and the pathologic type was moderately differentiated with complete resection margin. Considering the early stage of the cancer (pT1), and after the discussion with patient in multidisciplinary team, we decided not to proceeded adjuvant treatment and closely observe the recurrence of the tumor.
Because of the rarity, there are only few reports of auricle SCC in Korea [10-12]. Wide excision [10,11] and MMS [12] were previously used for surgical resection. For the reconstruction, chondrocutaneous advancement flap [11] and full thickness skin graft with local flap [12] was used. Due to the complex structure of anterior auricle, diverse local flap techniques has been introduced for better aesthetic outcome [13,14]. In this case, the patient was old aged and the amount of skin and soft tissue in preauricular area was much enough to fulfill the defect. We did not designed the retroauricular area based flap because the defect after the wide excision was not connected to the postauricular area and preauricular based rotatory flap had more advantage in shortening the distance of flap rotation. Moreover, preauricular area has sufficient vascular supply so the surgeon can safely design the flap with enough length and width. Concerning the postoperative scar, we made incision used in face-lift operation, which has the advantage in masking the scar. To the best of authors’ knowledge, there was no previous report using local rotatory buccal flap to reconstruct auricular defect after the wide excision of SCC. With the review of literatures, the authors report this case of local rotatory flap reconstruction after wide excision of primary auricular SCC.
Fig. 1.Preoperative findings. A: There was 1×1 cm sized single erythematic ulcerative lesion with crust on the cymba concha and antihelical rim (arrow). B: Axial view of temporal bone CT showed diffuse swelling of auricle and cartilaginous external auditory canal (EAC) (arrows). C: Axial view of T2 weighted MRI showed diffuse high signal intensity in right auricle and cartilaginous EAC (arrows). D: PET scan showed increased uptake in right auricle (white arrow) and mild uptake in right parotid gland (blue arrow). Fine needle aspiration biopsy result in parotid gland was benign. 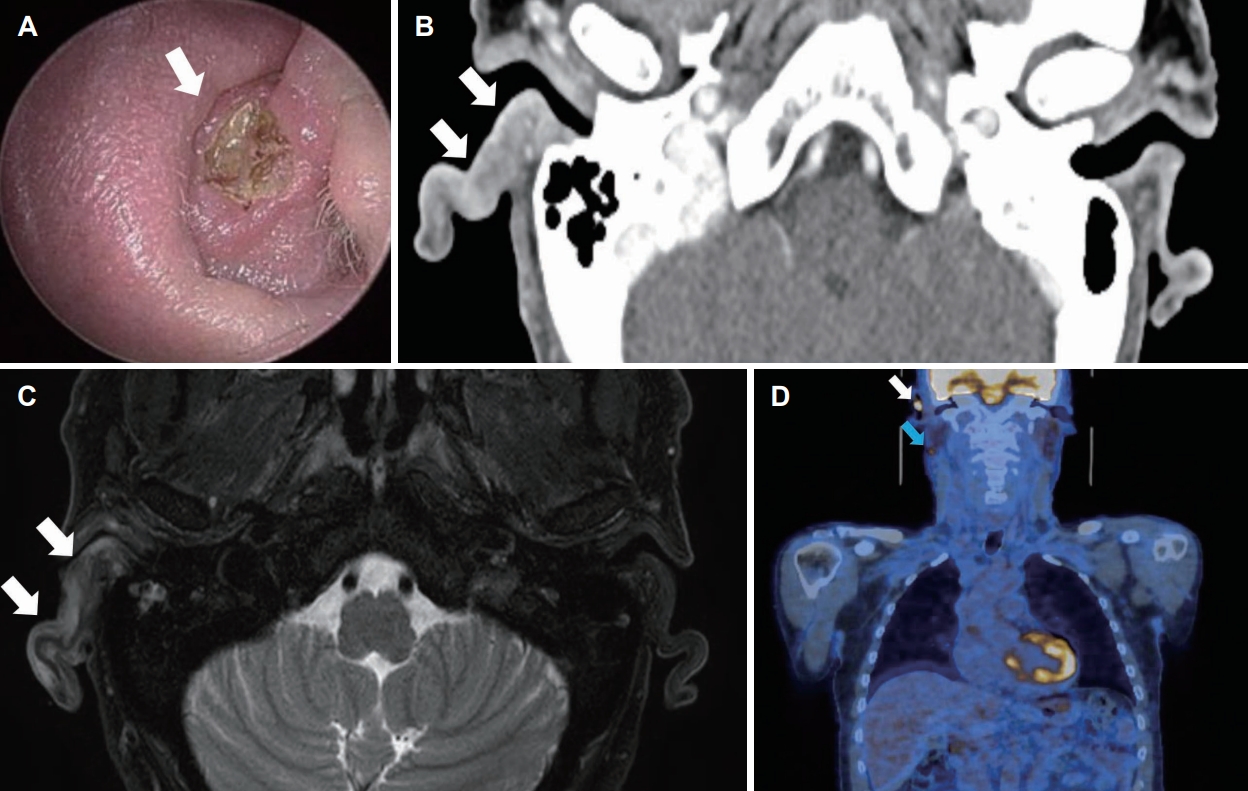
Fig. 2.Preoperative design of local flap. We designed local rotatory flap from buccal or temporal area. The volume of flap was measured based on the size of tumor (1×1 cm) and required safety margin (1 cm). “X” markings in the design are axis of the rotation. 
Fig. 3.Operation photograph. A: Horizontal width of the tumor was 1 cm and additional 1 cm of safety margin from the tumor was gathered. B: Vertical width of the tumor was 1.5 cm and additional 1 cm of safety margin from the tumor was gathered. C: Surgical photo after the wide excision. Pin in the specimen orientate the superior and inferior border of the excision margin. 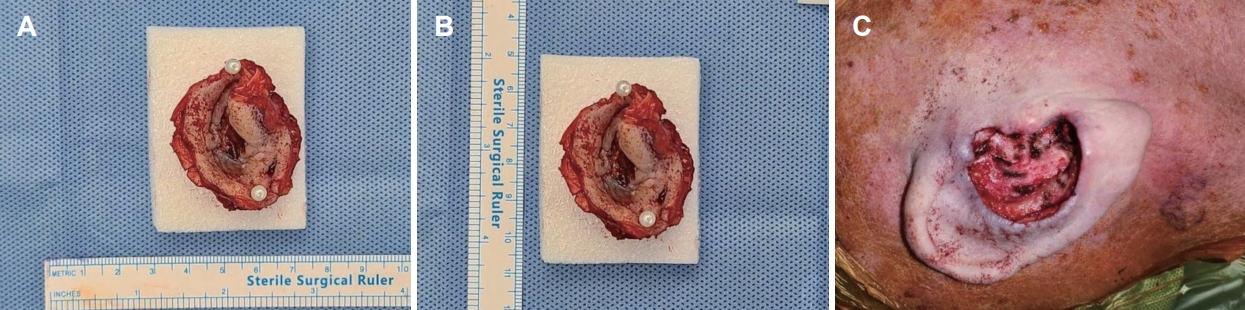
Fig. 4.Local flap coverage procedure. A: Flap design before elevation. “X” marking in the skin is location of feeding artery, which was used for the axis for roation. B: Elevation of flap over superficial musculoaponeurotic system layer. C: Rotation of flap to the defect. White and green arrow refers to the reconstruction of conchal area and helix crus, respectively. D: Photo of completed reconstruction. White, green, and blue arrow refers to the reconstructed conchal area, helix crus and external auditory canal inlet, respectively. 
Fig. 5.Pathologic finding. A: Cancer cells with pleomorphic nuclei (blue circle) were observed (hematoxylin and eosin [H&E], ×100). B: Partially keratinized pattern (red arrow) with pleomorphic cancer cells around the keratinization (red circle) were observed (H&E, ×400). C: Cytokeratin AE1/AE3 stain was diffusely positive (×200). 
Fig. 6. Postoperative 12 weeks photograph. A: Photograph of reconstructed right ear 12 weeks after the surgery. The local rotatory flap covered the defect stably while retaining its original shape. B: Photograph of the left ear. Aesthetic outcome of the operated right ear was satisfactory compared to the left ear. 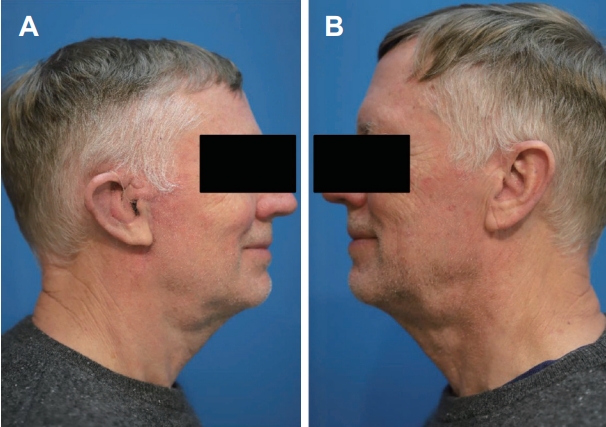
REFERENCES1. Silapunt S, Peterson SR, Goldberg LH. Squamous cell carcinoma of the auricle and Mohs micrographic surgery. Dermatol Surg 2005;31(11 Pt 1):1423-7.
2. Clark RR, Soutar DS. Lymph node metastases from auricular squamous cell carcinoma. A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg 2008;61(10):1140-7.
3. Kim JYS, Kozlow JH, Mittal B, Moyer J, Olenecki T, Rodgers P. Guidelines of care for the management of cutaneous squamous cell carcinoma. J Am Acad Dermatol 2018;78(3):560-78.
4. Mohs FE. Chemosurgical treatment of cancer of the nose; a microscopically controlled method. Arch Surg (1920) 1946;53:327-44.
5. Connolly SM, Baker DR, Coldiron BM, Fazio MJ, Storrs PA, Vidimos AT, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: A report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol 2012;67(4):531-50.
6. Chi FL, Gu FM, Dai CF, Chen B, Li HW. Survival outcomes in surgical treatment of 72 cases of squamous cell carcinoma of the temporal bone. Otol Neurotol 2011;32(4):665-9.
7. González A, Etchichury D, Rivero JM, Adamo L. Squamous cell carcinoma of the external ear: 170 cases treated with Mohs surgery. J Plast Reconstr Aesthet Surg 2021;74(11):2999-3007.
8. Harris BN, Pipkorn P, Nguyen KNB, Jackson RS, Rao S, Moore MG, et al. Association of adjuvant radiation therapy with survival in patients with advanced cutaneous squamous cell carcinoma of the head and neck. JAMA Otolaryngol Head Neck Surg 2019;145(2):153-8.
9. Stevenson ML, Criscito MC, Wilken R, Doudican NA, Bain EE 3rd, Parashar B, et al. Use of adjuvant radiotherapy in the treatment of high-risk cutaneous squamous cell carcinoma with perineural invasion. JAMA Dermatol 2020;156(8):918-21.
10. Kim CW, Kim CH, Lim YH, Nam ES. A case of keratoacanthoma-like squamous cell carcinoma of the auricle. Korean J Otorhinolaryngol-Head Neck Surg 2006;49(2):225-7.
11. Choi JH, Kim JY, Yoo YS, Cho KR. Chondrocutaneous advancement flap for helical rim defect. Korean J Otorhinolaryngol-Head Neck Surg 2010;53(4):252-5.
12. Yi KI, Kong SK, Goh EK, Oh SJ. Application of Mohs surgery to the treatment of basosquamous cell carcinoma originating from the auricle. Korean J Otorhinolaryngol-Head Neck Surg 2017;61(4):212-6.
|
|
|||||||||||||||||||||||||||||||||||||

 |
 |