 |
 |
AbstractBackground and ObjectivesWe evaluated the current status of percutaneous steroid injection (PSI) procedure for benign vocal fold lesions performed in Korea in order to achieve consensus about the indications, contraindications, anesthesia, complications, and the role of PSI.
Subjects and MethodAn email-based questionnaire survey consisting of 11 questions was administered to 20 experienced laryngologists.
ResultsThe most commonly used indication was small vocal nodule (32.7%). The most common contraindication was vocal fold lesion with atrophy (46.9%). Triamcinolone injection under local anesthesia by cricothyroid was usually used in the PSI procedure. Following the procedure, vocal fold atrophy was the most prominent complication (39.1%). The role of PSI is still not well established; however, most laryngologists considered it to be an adjunctive treatment (61.9%).
IntroductionBenign vocal fold lesions such as vocal nodules, polyps, and Reinke’s edema result from phonotrauma, chronic inflammation and subsequent remodeling of Reinke’s space [1-3]. Patients with small lesions require conservative treatment including voice therapy [1,4]. If the lesions are unresponsive to voice therapy or if the patients have recurrent disorders, laryngomicrosurgery (LMS) may be recommended for their removal. Voice therapy is limited by its relatively low compliance, long treatment period, and poor understanding on the part of the public regarding the voice therapy mechanism [3,5]. Additionally, LMS requires general anesthesia, with the increased possibility of dental problems [2,5]. Percutaneous steroid injection (PSI) for benign vocal fold lesions was introduced to fill the therapeutic gap between voice therapy and LMS [6].
Several studies have shown that PSI has considerable efficacy, compared to LMS and voice therapy [3,4,6,7]. If patients refuse standard treatments or their occupational/economic situations are not sufficient, PSI could be a useful alternative treatment modality. With a renewed interest in the advance of PSI, many laryngologists have worked to develop new approaches [3,5]. However, there is no established consensus about the indications, contraindications, anesthesia, or complications associated with PSI treatment. There is also no reliable survey on the various PSI techniques used by laryngologists.
Therefore, the aim of this study was to establish a general consensus about the indications, contraindications, anesthesia, complications, and their roles in PSI, based on the opinions of Korean laryngologists toward the development of guidelines for this approach in treating benign vocal fold lesions.
Subjects and MethodsBetween October and November 2019, an email-based survey was administered to 20 laryngologists with over 10 years of experience. In total, 8 tertiary hospitals, 2 secondary hospitals and 4 primary hospitals were included in the survey. The response rate was 100% (20/20). One laryngologist indicated that he did not perform the PSI procedure; thus, ultimately, 19 laryngologists completed the survey.
The survey consisted of 11 questions about the indications, contraindications, approach technique and anesthesia method during the PSI procedure, in addition to the complications, effectiveness, and recurrence, following the procedure. The participants were able to choose multiple responses or choose not to respond to the survey.
The survey questions included the following:
1. What do you consider to be the most effective indication(s) for the injection of steroids in the vocal folds?
2. What are your contraindication(s) for the procedure(s)?
3. Which material(s) do you use for PSI?
4. Which anesthesia method do you choose when you perform PSI?
5. How do you anesthetize the mucous membrane when performing PSI under local anesthesia?
6. Which approach do you prefer for the PSI procedure?
7. What do you think about the long-term effects of PSI?
8. What do you consider to be the role of the PSI technique in the future?
9. What do you consider to be the greatest disadvantages of PSI?
10. What do you do if vocal fold atrophy or vocal fold thinning occurs after PSI?
11. What do you consider to be the reason why vocal fold lesions recur after PSI?
ResultsIndications, contraindications and the materials used for the PSI procedureThe most common response for the most effective indications for PSI was that of small vocal nodule (32.7%), followed by mild-to-moderate Reinke’s edema (23.1%), small vocal polyp (15.4%), touch up procedure (PSI for recurrent small vocal nodules or polyps following LMS under general anesthesia) (13.5%), mild vocal fold scar (9.6%) (Fig. 1A). 2 laryngologists responded miscellaneous and described that PSI could be used as an adjuvant treatment for vocal cyst or secondary nodule during LMS under general anesthesia.
Contraindications for PSI included vocal fold lesion with vocal fold atrophy (46.9%), professional voice user (15.6%), large vocal polyp (15.6%), severe vocal fold scar (12.5%), and recurrence cases (9.4%) (Fig. 1B).
For materials used for percutaneous injection, 71.4% of laryngologists responded that triamcinolone acetonide (40 mg/mL; Shin Poong Pharm Co., Ltd, Seoul, South Korea) was injected, followed by dexamethasone disodium phosphate (5 mg/mL; Ilsung Pharm Co., Ltd, Seoul, South Korea) at 23.8% and injected miscellaneous materials at 4.8% (Fig. 2).
Anesthesia method and approach for the PSI procedureIn terms of the preferred anesthesia method for PSI, local anesthesia was most frequently used (61.1%). Some laryngologists selected anesthesia according to the patient’s situation such as general condition, underlying disease, compliance (33.3%), while others preferred general anesthesia (5.6%) (Fig. 3A).
In response to the question as to how laryngologists anesthetize the mucous membrane when performing PSI under local anesthesia, 33.3% responded that the oral cavity lidocaine spray alone was sufficient; 22.2% of laryngologists responded that lidocaine nebulizer, oral cavity lidocaine spray, and lidocaine laryngeal fold dripping were required; and 16.7% answered that a combination of oral cavity lidocaine spray and lidocaine nebulizer was needed. Some indicated that a lidocaine nebulizer, oral cavity lidocaine spray, laryngeal dripping, intravenous injection of midazolam, and tracheal lidocaine injection were required (11.1%), and 5.6% responded that lidocaine nebulizer, oral cavity lidocaine spray, laryngeal dripping, and intravenous injection of midazolam were needed. Some laryngologists indicated that the use of only a lidocaine nebulizer was enough (5.6%), while others felt that a superior laryngeal nerve block was sufficient (5.6%) (Fig. 3B).
The approach technique under local anesthesia included a cricothyroid approach (47.8%), a thyrohyoid approach (26.1%), a transoral approach (17.4%), a transcartilaginous approach (4.3%), and a combined approach (4.3%) (Fig. 4).
Long term effects and the future role of PSIAbout long term effects of PSI, 56.5% responded that it could be an adjuvant treatment, as compared to standard treatment, and 21.7% indicated that PSI was as effective as an independent treatment modality. Some laryngologists (21.7%) responded that PSI was not a verified procedure. However, none of the responders believed that PSI was not an effective treatment for benign vocal fold lesions (Fig. 5A).
Regarding the future role of PSI, 61.9% of laryngologists responded that it could be an adjuvant therapy with standard treatment, 33.3% responded that the procedure could be, independently, an effective technique, and 4.8% responded that it would play a very limited role and ultimately be replaced in the future (Fig. 5B).
Complications and recurrence of PSIThe most frequent response regarding complications was vocal cord atrophy (39.1%). Others indicated that there was no improvement after the procedure (26.1%) or suboptimal improvement (26.1%). The remainder of 8.7% listed vocal fold hematoma as one of the complications (Fig. 6).
To treat vocal fold atrophy after PSI, 61.1% of laryngologists responded that observation was enough. Other responses included voice therapy following the procedure (33.3%) and having additional injection laryngoplasty (5.6%). None of the laryngologists used medication to treat vocal fold atrophy (Fig. 7A).
When asked about the factors related to recurrence, persistent voice abuse was the one most reported by the respondents (46.2%), followed by heavy smoker (17.9%), large-size lesion (17.9%), throat clearing (12.8%), and professional voice user (5.1%) (Fig. 7B).
DiscussionGenerally, voice therapy and LMS are the standard treatments for benign vocal fold lesions. However, each treatment has its own limitations. Voice therapy requires multiple sessions to have an effect and shows low compliance in some patients, thus leading to LMS performed under general anesthesia [2,3,5]. To overcome these shortcomings, PSI has been introduced as a useful alternative modality for small vocal fold lesions [4,6,8]. Although PSI has been widely used due to its advantages, there is no consensus for indications, contraindications, method of anesthesia, or materials used with PSI treatment. There has also been no comparative study of the various PSI techniques.
Thus, it is important to collect and compare data from experienced laryngologists to understand the current situation and differences between the approaches. According to our survey, the triamcinolone injection under oral cavity lidocaine spray via the cricothyroid approach is the most preferred method. We assumed that oral cavity lidocaine spray is sufficient for suppressing the gag reflex due to its short procedure time, whereas the cricothyroid approach is preferable as surgeons can easily control the direction and location of the needles during the procedure. As triamcinolone agents are available as micronized suspensions for more efficient delivery to the treatment site, it is commonly used in PSI, compared to other steroid materials [9]. The dosage of steroid varies, but in South Korea, the majority injects 0.1 to 0.2 mL of triamcinolone acetonide (40 mg/mL) or dexamethasone disodium phosphate (5 mg/mL) per lesion without dilution [6].
For the indications and contraindications of PSI, 32.7% of laryngologists responded that small vocal nodules are an effective indication for the procedure, and 23.1% responded that mild-to-moderate Reinke’s edema is a possible indication. However, 46.9% answered that vocal fold lesion with atrophy is not a suitable indication for PSI. These results suggest that size and atrophy are important factors in determining whether PSI is possible.
For complications, 39.1% of laryngologists cited vocal fold atrophy after the procedure as the most frequent complication. The remaining side effects presented included no improvement (26.1%), suboptimal improvement (26.1%), and vocal fold hematoma (8.7%). When asked about the management of vocal fold atrophy, many laryngologists (61.1%) said careful observation was sufficient for the treatment. As recurrence occurred for persistent voice abuse (46.2%) and heavy smokers (17.9%), there were no serious complications of PSI such as dyspnea or vocal cord palsy.
The long-term effects of PSI have still not been established; some consider it to be an adjuvant treatment to standard treatment (56.5%) and others consider it effective as an independent treatment (21.7%) or that its effect cannot be verified (21.7%). The reason for the lack of established long-term effects of PSI is likely due to debates regarding its efficacy and recurrence rates. However, one study [6] previously reported the efficacy of PSI for benign vocal fold lesions, and Wang, et al. [3] found that the recurrence rates after PSI were between 4% and 31%. In terms of future role of PSI, 61.9% of laryngologists said PSI would be an adjuvant treatment, and 33.3% said it would be an effective independent treatment modality. Only 4.8% said that PSI would fade away in the future.
This study has limitation because this survey was performed with small 19-person. To optimize the usefulness of PSI, it is important to establish practical guidelines based on a strong consensus. We believe that a nationwide questionnaire survey about the PSI procedure is an important first step toward this goal.
In conclusion, there is therapeutic gap between voice therapy and LMS in South Korea. Our survey results provide a general consensus of opinions about PSI in an effort to establish guidelines for the indications, contraindications, anesthesia, complications, and their roles in this treatment modality. It is our hope that the results of our study provide insight into this alternative treatment strategy, thus filling a therapeutic gap for optimizing patient outcomes.
Supplementary MaterialThe Data Supplement is available with this article at https://doi.org/10.3342/kjorl-hns.2023.00549.
Supplementary Material Percutaneous steroid injection consensus survey
kjorl-hns-2023-00549-Supplementary-1.pdf
ACKNOWLEDGMENTSThis research was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning, South Korea (grant number: 2021R1I 1A3050685) and the Soonchunhyang University Research Fund.
This nationwide survey was performed among laryngologists who have experience in percutaneous steroid injection in South Korea. We thank them for their contributions. Tack Kyun Kwon, Department of Otolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul; Seong Keun Kwon, Department of Otolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul; Han Su Kim, Department of Otolaryngology-Head and Neck Surgery, Ewha Womans University, College of Medicine, Seoul; Young Ho Kim, Beautiful Voice Clinic, Seoul; Hyung Tae Kim, Yeson Voice Center, Seoul; Jun Hee Park, Department of Otolaryngology-Head and Neck Surgery, Chosun University School of Medicine, Gwangju; Jin Ho Sohn, Department of OtolaryngologyHead and Neck Surgery, School of Medicine, Kyungpook National University, Daegu; Cheol Min Ahn, PRANA ENT Clinic, Seoul; Seung Hoon Woo, Department of Otolaryngology-Head and Neck Surgery, Dankook University School of Medicine, Cheonan; Byung Joo Lee, Department of Otorhinolaryngology-Head and Neck Surgery and Biomedical Research Institute, Pusan National University Hospital, Busan; Sang Joon Lee, Department of Otolaryngology-Head and Neck Surgery, Dankook University School of Medicine, Cheonan; Jae Yol Lim, Department of Otolaryngology-Head and Neck Surgery, Yonsei University College of Medicine, Seoul; Sang Hyuk Lee, Department of Otorhinolaryngology-Head and Neck Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul; Jae Gu Cho, Department of Otorhinolaryngology-Head and Neck Surgery, Guro Hospital, Korea University College of Medicine, Seoul; Sung Min Jin, Department of Otorhinolaryngology-Head and Neck Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul; Won Jae Cha, Department of Otorhinolaryngology-Head and Neck Surgery and Biomedical Research Institute, Pusan National University Hospital, Busan; Yoon Seok Choi, Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, Yeungnam University, Daegu; Hong Shik Choi, HANA ENT Clinic, Seoul; Hyun Jun Hong, Department of Otorhinolaryngology-Head & Neck Surgery, International St. Mary’s Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea.
NotesAuthor Contribution Conceptualization: Seung Won Lee. Data curation: Shin Young Kim, Hyo-Jun Kim. Investigation: Shin Young Kim, Hyo-Jun Kim. Methodology: Seung Won Lee. Supervision: Seung Won Lee. Writing—original draft: Hyo-Jun Kim, Shin Young Kim. Writing—review & editing: Shin Young Kim, Seung Won Lee. Fig. 1.Indications and contraindications for percutaneous steroid injection. A: Indications for percutaneous steroid injection (PSI) in benign vocal fold lesions. B: Contraindications for PSI in benign vocal fold lesions. 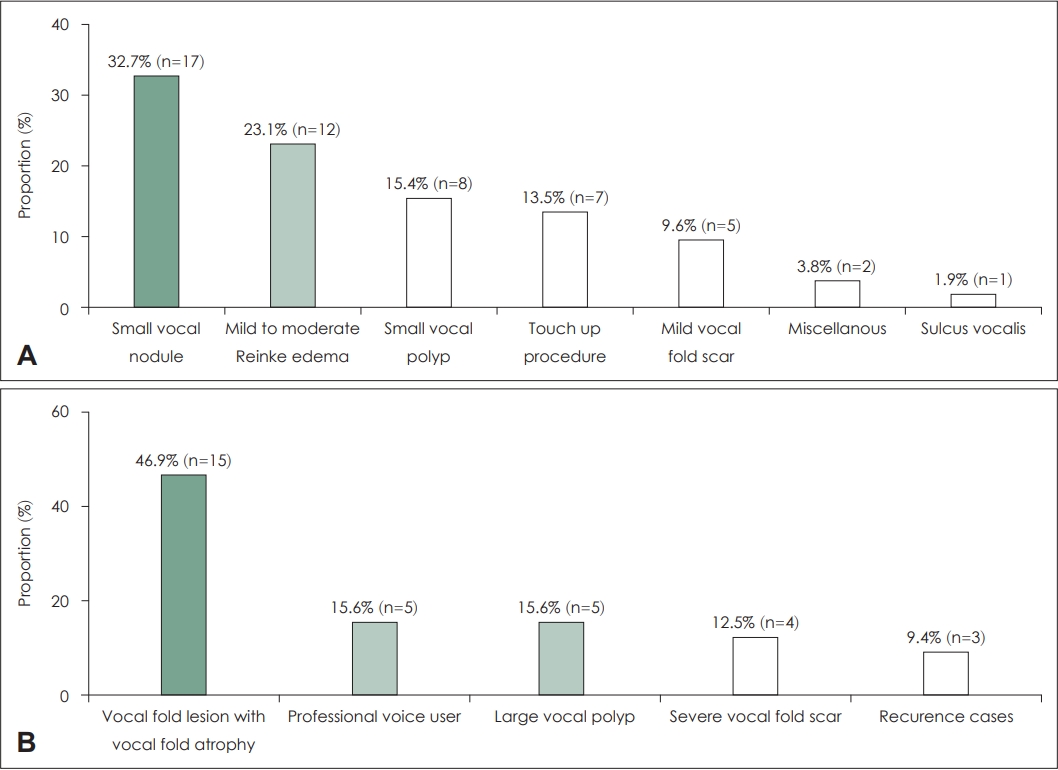
Fig. 3.Anesthesia methods for percutaneous steroid injection. A: Anesthesia method for percutaneous steroid injection (PSI) in benign vocal fold lesions. B: Currently used local anesthesia methods for PSI in benign vocal fold lesions. 
Fig. 4.Currently used approach techniques for percutaneous steroid injection in benign vocal fold lesions. 
REFERENCES1. Tateya I, Omori K, Kojima H, Hirano S, Kaneko K, Ito J. Steroid injection to vocal nodules using fiberoptic laryngeal surgery under topical anesthesia. Eur Arch Otorhinolaryngol 2004;261(9):489-92.
2. Martins RH, Fabro AT, Domingues MA, Chi AP, Gregório EA. Is Reinke’s edema a precancerous lesion? Histological and electron microscopic aspects. J Voice 2009;23(6):721-5.
3. Wang CT, Liao LJ, Cheng PW, Lo WC, Lai MS. Intralesional steroid injection for benign vocal fold disorders: A systematic review and meta-analysis. Laryngoscope 2013;123(1):197-203.
4. Tateya I, Omori K, Kojima H, Hirano S, Kaneko K, Ito J. Steroid injection for Reinke’s edema using fiberoptic laryngeal surgery. Acta Otolaryngol 2003;123(3):417-20.
5. Wang CT, Liao LJ, Lai MS, Cheng PW. Comparison of benign lesion regression following vocal fold steroid injection and vocal hygiene education. Laryngoscope 2014;124(2):510-5.
6. Woo JH, Kim DY, Kim JW, Oh EA, Lee SW. Efficacy of percutaneous vocal fold injections for benign laryngeal lesions: Prospective multicenter study. Acta Otolaryngol 2011;131(12):1326-32.
|
|
|||||||||||||||||||||||||||||||||||||||||

 |
 |