 |
 |
AbstractBackground and ObjectivesCognitive behavioral therapy (CBT) is a treatment option for subjective tinnitus. There are many reports on its clinical efficacy, but the protocol has not been well established. The purpose of this study was to set an outpatient-based CBT protocol and evaluate its clinical efficacy for tinnitus.
Subjects and MethodA total of 85 chronic tinnitus patients was assessed in this prospective study. After evaluating for eligibility, 30 patients completed CBT based on a protocol of 5 weekly sessions in an outpatient setting. Therapeutic efficacy was assessed by Tinnitus Handicap Inventory (THI) questionnaires and visual analogue scale (VAS) for tinnitus. The initial scores were compared with the final scores, which were assessed a month after the fifth CBT session.
IntroductionTinnitus is a common auditory symptom characterized by the perception of sound in the absence of an external acoustic stimulus. It affects millions of people worldwide, and while it is not a life-threatening condition, it can significantly impact quality of life [1]. Tinnitus can cause negative emotional reactions such as insomnia, difficulty concentrating, communication problems, anxiety and depression [2]. It is known that nearly 20% of the total population experiences tinnitus globally, and 1% to 3% of them complain of symptoms that cause discomfort in daily life [3,4].
There are various treatments for tinnitus, such as sound therapy, tinnitus retraining therapy, and drugs such as antianxiety and antidepressants, but none of these treatments have been proven to cure tinnitus. The patients’ satisfaction with current tinnitus treatment methods is unsatisfactory. Cognitive behavioral therapy (CBT) was first developed by Beck and was initially applied to depression, and then insomnia, chronic pain, and anxiety disorders and Sweetow first introduced CBT to tinnitus [2,5,6]. The main concept of CBT is that negative and unrealistic cognition causes maladaptive behavior. By correcting these negative perceptions, patients can treat tinnitus by having more positive and realistic thinking [7,8]. CBT for tinnitus mainly focuses on reducing the pain and disability caused by tinnitus. There are reports that supports the therapeutic efficacy of CBT but there is no consensus for clinical protocol yet. In addition, traditional CBT treatment usually provides a variety of contents over a long period of time, focusing on the correction of cognitive distortions through counseling for more than three months [9]. Since it is difficult to conduct such long-term treatment in reality in Korea, the authors applied a program suitable for the domestic medical environment, focusing on cognitive distortion.
This primary goal of this study is to analyze the treatment efficacy of outpatient-based CBT protocol for tinnitus patients by using the Tinnitus Handicap Inventory (THI) and visual analogue scale (VAS). The journal will also discuss the theoretical basis, treatment components, challenges and limitations of CBT, and provide suggestions for future research in this area.
Subjects and MethodsStudy participantsA total of 85 tinnitus patients were treated with CBT between January 2021 and September 2022, from a tertiary health care center in Korea. Chief complaint of continuous, chronic subjective tinnitus for at least 6 months, a score of ≥18 in the THI (at least mild tinnitus distress), ability to participate in all relevant visits, age over 18 and less than 90 without any cognitive or systemic diseases were the inclusion criteria in this study. All patients completed otolaryngologic examination. Patients with perforation of the tympanic membrane, otalgia, otorrhea, and cognitive disorder, sudden hearing loss, severe or profound hearing loss, patient with hearing aid, heart disease, and patient who did not complete all sessions were excluded from the study. Among 85 patients, 55 patients were excluded for not meeting the eligibility. Seven patients had severe or profound hearing loss, five patients had heart disease, two patients had cognitive disorder with dementia, and 41 patients dropped out during sessions mostly due to physical difficulties (34) and rest for unknown reasons (7). The medications the patients were taking prior to treatment were maintained. The study was performed in accordance with the Helsinki Declaration. The Institutional Review Board of the Korea University Guro Hospital approved this study (IRB No. 2021GR1450005).
Treatment protocolThis protocol provides educational content centered on correcting cognitive distortions that patients have about tinnitus. Depending on the patient, these include sleep education, relaxation therapy, imagery training, and positive thinking. A thought record sheet was provided so that people could record when they hear tinnitus during the day, what emotions and thoughts they have when they hear tinnitus, and correct and record these thoughts in a positive way. This is later received through consultation with the doctor during outpatient treatment (Fig. 1).
A total of 5 consultation sessions were done weekly. The patient was visited once a week, and a consultation with the clinician was done for about 20 minutes for each session. At the beginning of the consultation, a tinnitus treatment record sheet was given to the patient to record the thoughts of tinnitus in their daily life. On the next visit, the clinician reviewed the tinnitus treatment record written by the patient, and based on this, counseling was conducted on every visit session by physician (Fig. 2).
The patient’s THI and a VAS for loudness and duration of tinnitus were recorded at the beginning and end of the CBT treatment, and VAS for negative thoughts, negative emotions were checked on every visit along with tinnitus record sheet (Fig. 3).
QuestionnaireThe THI is a 25-item tool questionnaire widely used worldwide to evaluate the discomfort caused by tinnitus or to verify the effectiveness of treatment. Each question was numbered as 0 (no problem), 2 (sometimes), and 4 (severe) and total score ranged from 0-100. The THI can provide valuable information about the subjective impact of tinnitus on a patient’s life, and it has been shown to be a reliable and valid measure of tinnitus-related distress [10]. Tinnitus improvement was considered as 20-point reduction in total THI score. Patients completed THI survey form before and after the CBT treatment.
The VAS is a rating scale (0-10) in which subjects subjectively rate their health outcomes and mark them along a printed line [11]. The VAS is a simple and quick method for assessing the subjective loudness and annoyance of tinnitus. Patients are asked to rate the loudness and annoyance of their tinnitus on a scale of 0 to 10, with 0 indicating no tinnitus and 10 indicating the loudest and most annoying tinnitus imaginable. Patients rated VAS score for negative thought, negative emotions on every session, VAS score for loudness and duration at the beginning of CBT treatment and end of the treatment.
ResultsBaseline characteristicsThe study patients consisted of 11 males and 19 females, and the average age was 60 years old. Seventeen patients had unilateral tinnitus and 13 patients had bilateral tinnitus. All patient’s audiometry was either mild or moderate hearing loss. The average hearing threshold was 30.5 dB for right and 26.9 dB for left. Patients suffered tinnitus for 6.2 years in average (Table 1).
THI score differenceThe total THI score at initial of CBT was (55.8±25.7), and score decreased to (24.0±17.0) at final, tinnitus improvement was seen in 70.0% (n=21) of patients, which was statistically significant (p<0.05). The functional score, emotional score, and catastrophic scores were (23.5±11.8), (22.3±10.4), and (10.0±6.3) at initial. These scores decreased to (10.1±8.8), (9.9±7.3), and (4.0±4.1) (Table 2).
VAS score differenceBefore the CBT, the average VAS score for negative thoughts about the tinnitus was (6.0±2.3), The VAS score continued to decrease from the beginning of the CBT to the second (4.5±2.2), third (4.1±1.9), fourth (3.2±1.7), and fifth session (2.7±1.7), and showed a statistically significant decrease from the second session compared to the initial value (p<0.05).
The initial VAS score for negative emotion about the tinnitus was (6.3±2.2). Emotion VAS score also continued to decrease from initial to the second (4.5±1.8), third (4.4±2.3), fourth (3.4±1.9), and fifth session (2.7±1.6), and showed a statistically significant decrease from the third session compared to the initial value (p<0.05) (Fig. 4).
The initial VAS for subjective loudness was (7.2±1.3) and initial frequency of tinnitus was (7.4±1.7). The final VAS for loudness was (4.2±1.9) and final frequency VAS was (4.8±2.6). The decrease in VAS score was statistically significant (p<0.001) (Fig. 5).
DiscussionThe 4-week 5-session CBT protocol was clinically meaningful for tinnitus patients which was assessed by THI and VAS score. As a result, when comparing before and after treatment, both the THI and VAS score decreased significantly.
Tinnitus can cause a small, mild level of discomfort to a significant discomfort that interferes with daily life. The degree of discomfort caused by tinnitus felt by the patient is not directly related to the size of the tinnitus, so even very small tinnitus can cause discomfort in daily life, which can result in various symptoms such as anxiety and difficulty concentrating [12].
There is a difference between CBT and tinnitus retraining treatment (TRT) in the treatment of tinnitus. TRT is based on the premise that the patient’s tinnitus and negative emotions are conditioned by the conditioned reflex, and directive counseling is performed as a way to decondition them. It is emphasized not to think about it [13]. On the other hand, in CBT, the main purpose is to correct these cognitive distortions under the premise that the patient’s negative emotions caused by tinnitus are caused by false thoughts (cognitive distortions) about tinnitus. Therefore, the goal of counseling is not to induce people to forget and not think about tinnitus, but to have the insight that even if they have tinnitus, they can get along well, and that the wrong thoughts about tinnitus based on excessive worry and fear may be the cause of their hardship.
CBT involves a collaborative approach where the patient and therapist examine the patient’s fearful thoughts as hypotheses to be tested. This is done by understanding the link between thoughts and feelings and identifying the core beliefs that maintain these thoughts. CBT aims to reduce the pain and anxiety caused by tinnitus [14]. CBT for tinnitus typically involves several treatment components, including psychoeducation, cognitive restructuring, relaxation training, and behavioral activation. Psychoeducation aims to provide patients with accurate information about tinnitus and its causes, as well as strategies for managing tinnitus-related distress. Cognitive restructuring involves identifying and challenging negative thoughts and beliefs about tinnitus and replacing them with more adaptive and realistic ones. Relaxation training aims to reduce physiological arousal and promote relaxation, which can help to reduce tinnitus-related distress. Behavioral activation involves encouraging patients to engage in activities they enjoy and find meaningful, even if they are experiencing tinnitus-related distress. Likewise, its main goal is to alleviate the discomfort caused by distorted thoughts by reconstructing them into more positive and realistic thoughts [15]. According to the multidisciplinary European guideline in 2019 for tinnitus, CBT is considered as an effective and safe treatment with high-level of evidence [16].
THI is used to quantify the impact of tinnitus on daily living in three subscales - functional, emotional and catastrophic. An improvement in the THI score indicates the improvement of distress due to tinnitus in daily [11]. Although there are previous studies that CBT showed improvements of distress like negative thoughts and emotions caused by tinnitus, it was questionable whether it reduced the tinnitus loudness or its duration. A study by Andersson and Lyttkens [17] found that CBT had a moderate effect in controlling the discomfort caused by tinnitus, but showed a relatively less effect in reducing the size of tinnitus. In the analysis of Martinez-Devesa, et al. [18], CBT did not show a change in the subjective size of tinnitus, but the quality of life was significantly increased comparted to control. In our study, the both loudness and duration of tinnitus were reduced after CBT significantly.
Tinnitus is caused by various pathophysiologic pathways that cannot be explained by a single mechanism. Recently, De Ridder, et al. proposed a new triple brain cortical network model to explain complex mechanism of tinnitus: the ascending lateral sound pathway for loudness, the ascending medial pathway for suffering, and a descending noise-canceling pathway for duration of tinnitus [19,20]. Considering that CBT showed effects on loudness, duration, negative thoughts, or emotions in this study, it can be seen that CBT affects all three cortical networks.
According to Cochrane data systemic review, there is no established protocol for CBT for tinnitus patients. CBT approaches differ in number of sessions, hours spent for consultation, group versus individual, face-to-face versus online or combination. Several randomized controlled trials have demonstrated the effectiveness of CBT for tinnitus, with significant reductions in tinnitus-related distress and improvements in quality of life reported following treatment. However, there are also some challenges and limitations to CBT for tinnitus, including difficulties with patient engagement and adherence, the need for individualized treatment, and the potential for relapse following treatment. Also, there is yet no standardization of outcome selection to evaluate treatment efficacy [9]. It usually consists of five to ten weekly therapy sessions, either one-on-one or in small groups. Each session focuses on a particular topic, such as providing an understanding of tinnitus, strategies to improve sleep quality, stress management techniques, relaxation methods, and cognitive restructuring exercises [21]. There were studies on CBT without face-to-face sessions. Kaldo, et al. [22] found significant improvements in tinnitus anxiety, insomnia, and depression on the Tinnitus Reaction Questionnaire in a 7-week CBT treatment using a self-help book and telephone support method. Kaldo, et al. [23] evaluated tinnitus distress between standard group-based CBT and internet-based CBT and found that the Internet treatment was 1.7 times as cost-effective as the group treatment with a similar outcome.
In this study, the authors made a simple outpatient-based protocol of CBT for tinnitus and applied it to clinical treatment. Referring to the fact that most of the existing protocols consisted of 5 to 10 sessions, this protocol consisted of 5 sessions. Consultation was conducted face-to-face by a physician, and the THI and VAS questionnaires were evaluated one month after the end of treatment. Existing protocols made judgments immediately, after 1 month or 6 months to 12 months, for evaluation of treatment effect. Henry, et al. [24] reported that the treatment effect of CBT diminished after 12 months. Further studies on the long-time effect will be needed in the future. This study is expected to promote follow-up studies in that it has provided the basis for CBT treatment for tinnitus in the future. As a limitation of this study, this protocol requires 5 visits over 4 weeks, which may be physically difficult for patients to visit regularly. In fact, more than half of the patients dropped out of this study, and most of them were due to physical difficulties. Therefore, subjects with relatively high compliance who did not drop out were selected as a study group. CBT can also be seen as requiring continuous treatment. Digital-based treatment, a method that does not require patients to visit a medical institution every time, may be helpful. Also, there was no control group to compare the results with other treatment methods. Further studies on long-term prognosis with a larger number of patients with control group will be needed in the future.
To conclude, an outpatient-based CBT protocol for tinnitus was applied to the tinnitus patients. After CBT treatment, THI and VAS for negative thoughts and emotions related to tinnitus showed a statistically significant decrease. Therefore, outpatient-based CBT is a good treatment option for tinnitus.
NotesAuthor contributions Conceptualization: Jong-Geun Lee, Jae-Jun Song. Data curation: Jong-Geun Lee, Yongmin Cho, Hyunseok Choi, Gi Hwan Ryu, Jaeman Park, Dongha Kim. Formal analysis: Jong-Geun Lee, Yongmin Cho, Sung-Won Chae. Investigation: Hyunseok Choi, Sung-Won Chae, Jae-Jun Song. Methodology: Gi Hwan Ryu, Jong-Geun Lee, Sung-Won Chae, Jae-Jun Song. Project administration: Sung-Won Chae, Jae-Jun Song. Supervision: Jae-Jun Song. Validation: Sung-Won Chae, Jae-Jun Song. Visualization: Jong-Geun Lee. Writing— original draft: Jong-Geun Lee. Writing—review & editing: Jong-Geun Lee, Jae-Jun Song. Fig. 1.Tinnitus treatment record sheet. A: Tinnitus treatment record sheet in English. B: Example of tinnitus treatment record sheet from patient. 
Fig. 2.Scheme of CBT protocol. CBT, cognitive behavioral therapy; THI, Tinnitus Handicap Inventory; VAS, visual analogue scale. 
Fig. 3.Visual analogue scale (VAS) survey form for VAS-T, VAS-E, VAS-L, and VAS-D. VAS-T, VAS for negative thoughts; VAS-E, VAS for negative emotions; VAS-L, VAS for loudness; VAS-D, VAS for duration (the original form was in Korean, this is an English translation). 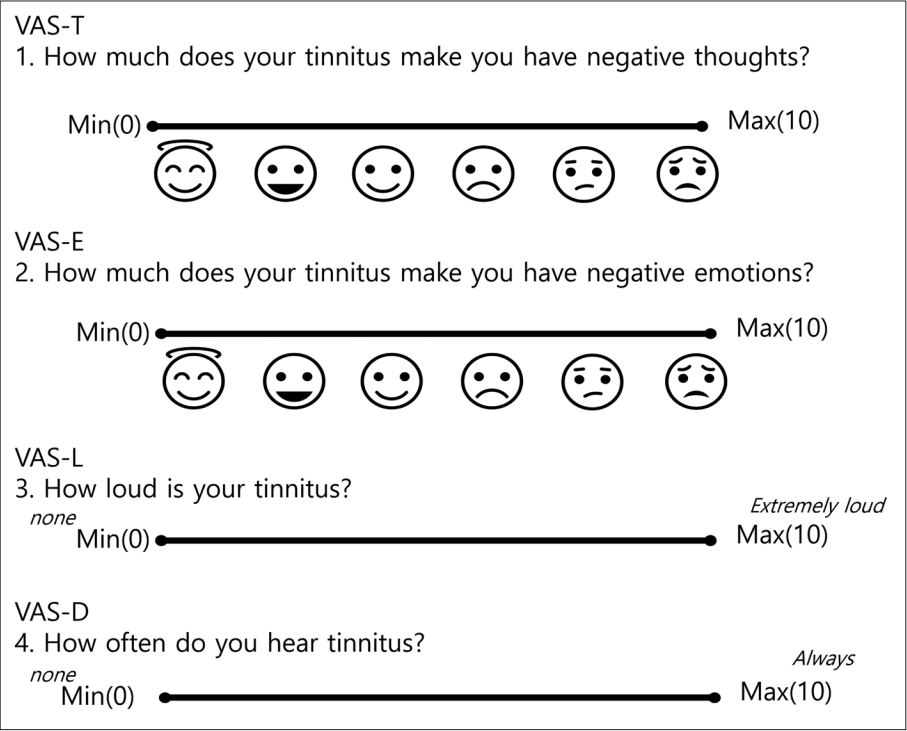
Fig. 4.Thought and emotion visual analogue scale (VAS) survey result. A: Negative thought VAS. B: Negative emotion VAS. *p<0.05; **p<0.001; compared to initial. 
Fig. 5.Loudness and duration visual analogue scale (VAS) survey result. For loudness, score 0 is considered as none and 10 as extremely loud. For duration, score 0 is considered as none and 10 as always. **p<0.001; compared to initial. 
Table 1.Baseline characteristics (n=30) REFERENCES1. Hoare DJ, Edmondson-Jones M, Sereda M, Akeroyd MA, Hall D. Amplification with hearing aids for patients with tinnitus and co-existing hearing loss. Cochrane Database Syst Rev 2014;1:CD010151.
2. Rush AJ. At the research front: Cognitive therapy for depression. Aust N Z J Psychiatry 1979;13(1):13-6.
3. Heller AJ. Classification and epidemiology of tinnitus. Otolaryngol Clin North Am 2003;36(2):239-48.
4. Axelsson A, Ringdahl A. Tinnitus--a study of its prevalence and characteristics. Br J Audiol 1989;23(1):53-62.
6. Beck AT. Cognitive therapy: Nature and relation to behavior therapy. J Psychother Pract Res 1993;2(4):342-56.
7. Zenner HP, Pfister M, Birbaumer N. Tinnitus sensitization: Sensory and psychophysiological aspects of a new pathway of acquired centralization of chronic tinnitus. Otol Neurotol 2006;27(8):1054-63.
8. Greimel KV, Kröner-Herwig B. Cognitive behavioral treatment (CBT). In: Møller AR, Langguth B, DeRidder D, Kleinjung T, eds. Textbook of Tinnitus. New York: Springer; 2011. p. 557-61.
9. Fuller T, Cima R, Langguth B, Mazurek B, Vlaeyen JW, Hoare DJ. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev 2020;1:CD012614.
10. Newman CW, Jacobson GP, Spitzer JB. Development of the tinnitus handicap inventory. Arch Otolaryngol Head Neck Surg 1996;122(2):143-8.
11. Torrance GW, Feeny D, Furlong W. Visual analog scales: Do they have a role in the measurement of preferences for health states? Med Decis Making 2001;21(4):329-34.
12. König O, Schaette R, Kempter R, Gross M. Course of hearing loss and occurrence of tinnitus. Hear Res 2006;221(1-2):59-64.
13. Phillips JS, McFerran D. Tinnitus retraining therapy (TRT) for tinnitus. Cochrane Database Syst Rev 2010;2010(3):CD007330.
14. Westin VZ, Schulin M, Hesser H, Karlsson M, Noe RZ, Olofsson U, et al. Acceptance and commitment therapy versus tinnitus retraining therapy in the treatment of tinnitus: A randomised controlled trial. Behav Res Ther 2011;49(11):737-47.
15. Beck JS. Cognitive behavior therapy: basics and beyond. 2nd ed. New York: Guilford Press; 2011.
16. Cima RFF, Mazurek B, Haider H, Kikidis D, Lapira A, Noreña A, et al. A multidisciplinary European guideline for tinnitus: Diagnostics, assessment, and treatment. HNO 2019;67(Suppl 1):10-42.
17. Andersson G, Lyttkens L. A meta-analytic review of psychological treatments for tinnitus. Br J Audiol 1999;33(4):201-10.
18. Martinez-Devesa P, Perera R, Theodoulou M, Waddell A. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev 2010;9:CD005233.
19. Menon V. Large-scale brain networks and psychopathology: A unifying triple network model. Trends Cogn Sci 2011;15(10):483-506.
20. De Ridder D, Vanneste S, Song JJ, Adhia D. Tinnitus and the triple network model: A perspective. Clin Exp Otorhinolaryngol 2022;15(3):205-12.
21. Andersson G. Psychological aspects of tinnitus and the application of cognitive-behavioral therapy. Clin Psychol Rev 2002;22(7):977-90.
22. Kaldo V, Cars S, Rahnert M, Larsen HC, Andersson G. Use of a self-help book with weekly therapist contact to reduce tinnitus distress: A randomized controlled trial. J Psychosom Res 2007;63(2):195-202.
|
|
|||||||||||||||||||||||||||||||||||||||||

 |
 |