 |
 |
AbstractA posterior tracheal wall rupture is a rare but life-threatening complication of tracheostomy. Several flaps based on the sternocleidomastoid (SCM) muscle, which has sufficient length and abundant blood supply, are utilized for the reconstruction of tracheal defects. We discuss here a case of a 71-year-old male with multiple organ failure and mental retardation, with posterior tracheal wall damage that had occurred during tracheostomy tube insertion. When planning the repair of the wound, additional reinforcement was necessary due to saliva leakage secondary to decreased consciousness. Direct suturing was followed by the reinforcement of SCM muscle transposition, which was conducted through cervical and endoscopic approach.
IntroductionThe posterior wall of the trachea consists of a membranous structure, and iatrogenic damage is reported to rarely occur during tracheal intubation, percutaneous tracheostomy, or surgical tracheostomy [1-3]. Repairs of injuries include suturing through an intraluminal approach using a bronchoscope [4], or suturing through a tracheostomy hole [2]. It can also be resolved by a cervical approach. In most cases, primary suture is used, but if the defect is small, there are cases where a muscle transposition flap after vascular transposition is used instead of primary suture [5].
Among the various structures employed for cervical reconstruction, the utilization of the sternocleidomastoid (SCM) muscle stands as the primary method for addressing tracheal damage [6], The myocutaneous flap, using the skin attached to the SCM muscle [7], and the myoperiosteal flap, using ostium attached to the SCM muscle at the clavicle level, are commonly used [8]. This is attributed to the advantages of significant muscle mobility, ample length, and the ability to use attached skin or periosteum as material for restoring the mucosal membrane.
We aim to share our successful case of repairing posterior wall damage occurring during tracheostomy by repositioning the SCM muscle, in a patient with ongoing saliva aspiration into the trachea.
CaseThis patient is a 71-year-old male with a medical history that includes tuberculosis treatment 40 years ago, early gastric cancer 4 years ago, and lung cancer 1 year ago.
This patient underwent an endoscopic submucosal dissection to remove multiple polyps observed during a colonoscopy performed 3 years ago. However, 4 days later, the patient presented with abdominal pain, leading to further examination and a diagnosis of sigmoid colon perforation. Subsequently, the patient underwent Hartmann’s procedure in the general surgery department. Over the following 2 months, intra-abdominal infection and pneumonia were confirmed, resulting in high fever and respiratory depression. In the impression of sepsis, tracheal intubation was performed. Despite maintaining endotracheal intubation (E-tube) and continuous monitoring in the intensive care unit (ICU), the patient’s consciousness did not significantly improve, prompting anticipation of prolonged E-tube. Consequently, a tracheostomy was planned and delegated to the otolaryngology department.
The tracheostomy was performed in the standard fashion, a transverse incision between the second and third tracheal cartilages was made. However, severe calcification of the tracheal cartilage at the level of the thyroid isthmus caused significant resistance and delayed insertion of the tracheostomy tube after the procedure. Immediately after intubation, however, mechanical ventilation was not functioning properly. Upon inserting a flexible bronchoscope into the tracheostomy tube, it was observed that the tip of the tracheostomy tube was positioned within the soft tissue, not within the tracheal lumen. Based on these findings, damage to the posterior wall of the trachea was suspected. The tracheostomy tube was removed, and the patient was switched to E-tube through the oral cavity. A subsequent CT scan revealed damage to the posterior tracheal wall and pneumomediastinum (Fig. 1). To slow the worsening of mediastinal emphysema due to positive pressure ventilation, the end of the E-tube was placed distally, below the suspected area of injury in the posterior tracheal wall. After that, significant amount of saliva was observed flowing through the tracheostomy site due to aspiration associated with the patient’s altered consciousness. Due to the patient’s consciousness level and the necessity for observations in the ICU, tests to confirm esophageal damage were not conducted.
Four days after the tracheal fenestration, we planned a revision tracheostomy to assess the degree of damage to the posterior tracheal wall and to repair it. Initially, the revision tracheostomy aimed to widen the previous tracheostomy hole, which had not been sufficiently enlarged, ensuring no resistance during the insertion of the tracheostomy tube. Thereafter, mechanical ventilation was temporarily halted, and the orally inserted E-tube was positioned above the tracheostomy hole. An endoscope was then inserted into the tracheostomy hole, confirming posterior wall damage (Fig. 2). The size of the damage was more than 2.5 cm in length and 1 cm in width, and it was verified that there was no damage to the esophageal adventitia located just below the posterior wall of the trachea.
In general, stability after repairing posterior tracheal wall damage can be ensured by placing the E-tube balloon more distally than the damaged area after suturing. However, in this case, a significant amount of saliva had already been aspirated into the trachea, necessitating the reinforcement of the posterior tracheal wall. Therefore, through a cervical approach, the larynx and trachea were separated from the surrounding soft tissue, rotated more than 90 degrees, and the posterior wall of the trachea was directly sutured with Vicryl 4-0. Subsequently, additional suturing for the tracheal inner wall was performed under endoscopic guidance through the tracheostomy hole (Fig. 3). Finally, the posterior wall was reinforced by relocating the SCM muscle. A superior-based SCM muscle flap was prepared; the sternal head of the SCM muscle were cut. And the left thyroid lobe was separated from the trachea and dissected laterally with the surrounding tissue hugging the trachea closely and placing laterally to avoid injuring the recurrent laryngeal nerve. After placing the prepared SCM muscle between the trachea and the left thyroid lobe, it was brought out through the lower part of the right thyroid lobe and then sutured to the medial aspect of the right SCM muscle (Fig. 3).
After the completion of the surgery, the wound area was regularly examined, and the follow-up CT scan revealed improvement in mediastinal emphysema. Additionally, the amylase level in the right pleural fluid was not elevated, indicating no saliva leakage up to 2 months after surgery (Fig. 4).
DiscussionTracheostomy is generally considered a safe procedure, with potential complications including surgical site infection, tracheomalacia, skin damage, tracheoesophageal fistula, bleeding, tracheostomy tube dislocation, and tracheostomy tube obstruction [9,10]. Among these, damage to the posterior wall of the airway is rare and has been reported in percutaneous dilatational tracheostomy [11]. In general surgical tracheostomy, tracheoesophageal fistula may occur due to the pressure of the E-tube balloon, but its frequency has been reported to be very low at 0.01% [12].
The reason why damage to the posterior wall of the airway rarely occurs in surgical tracheostomy may be attributed to the ability to insert the tracheostomy tube under a sufficient visual field through the tracheostomy hole. However, in this case, excessive force was applied to insert the tracheostomy tube without ensuring a sufficiently sized tracheostomy hole, resulting in posterior tracheal wall damage. In cases of simple posterior wall damage, internal suturing using an already created tracheostomy hole and placing the tip of the tracheostomy tube or E-tube distally to the damaged area can be expected to improve the injury site by preventing air leaks from positive pressure ventilation. However, in this case, it was deemed that additional reinforcement would be necessary due to the aspiration of saliva.
For the operation, the interposition of the SCM muscular flap was carried out in a manner consistent with previously reported methods [13]. And a cervical approach was employed to open the posterior pharyngeal space [14]. This aided in performing suturing while visually confirming the damage to the tracheal wall. However, in this patient, securing an adequate surgical view was challenging due to the damaged area being located at the level of the sternum. It was difficult to suture the inner tracheal wall altogether, so additional suturing was performed through the tracheostomy hole under endoscopic guidance. Subsequently, the SCM muscle was placed between the trachea and esophagus to successfully provide additional reinforcement. While it remains unclear whether repositioning the SCM muscle actively contributed to defending against wound damage from saliva, successful reinforcement of damaged areas using the SCM or strap muscle in tracheal perforation cases suggests a potential role in wound recovery in this instance [5,15].
This case underscores that damage to the posterior wall of the trachea is one of the possible complications in surgical tracheostomy. Among various methods to repair it, using the SCM muscle can serve as a method for additional reinforcement alongside primary repair. Above all, the prevention of complications such as damage to the posterior tracheal wall is crucial. In surgical tracheostomy, creating a tracheal stoma of sufficient size is imperative, and caution should be exercised to avoid excessive insertion of a tracheostomy tube, which can lead to potentially fatal problems.
ACKNOWLEDGMENTSThe study protocol was reviewed and approved by the Institutional Review Board of Seoul National University Hospital, which granted a waiver of informed consent. Approval was given for the purpose of case report (IRB No. H-2401-050-1500).
Fig. 1.Postoperative neck contrast-enhanced CT, 1 day after tracheal fenestration, revealed a posterior tracheal wall injury (arrow) and elongated air between the trachea and esophagus (asterisk), indicating pneumomediastinum. 
Fig. 2.Intraoperative endoscopic image taken 4 days after tracheal fenestration. The size of the damage measured more than 2.5 cm in length and 1 cm in width, with no definite injury to the esophageal adventitia (E, esophageal adventitia) observed. 
Fig. 3.Endoscopic photos and schematic images of the surgical treatment process. After suturing the outer membrane using a cervical approach (A), the inner layer was sutured using a tracheostomy (B). Following the separation of the left thyroid from the trachea, the left sternocleidomastoid muscle was dissected at the level of the clavicle (C). The dissected muscle was positioned between the trachea and the left thyroid lobe (D), then brought out through the lower part of the right thyroid lobe (E). 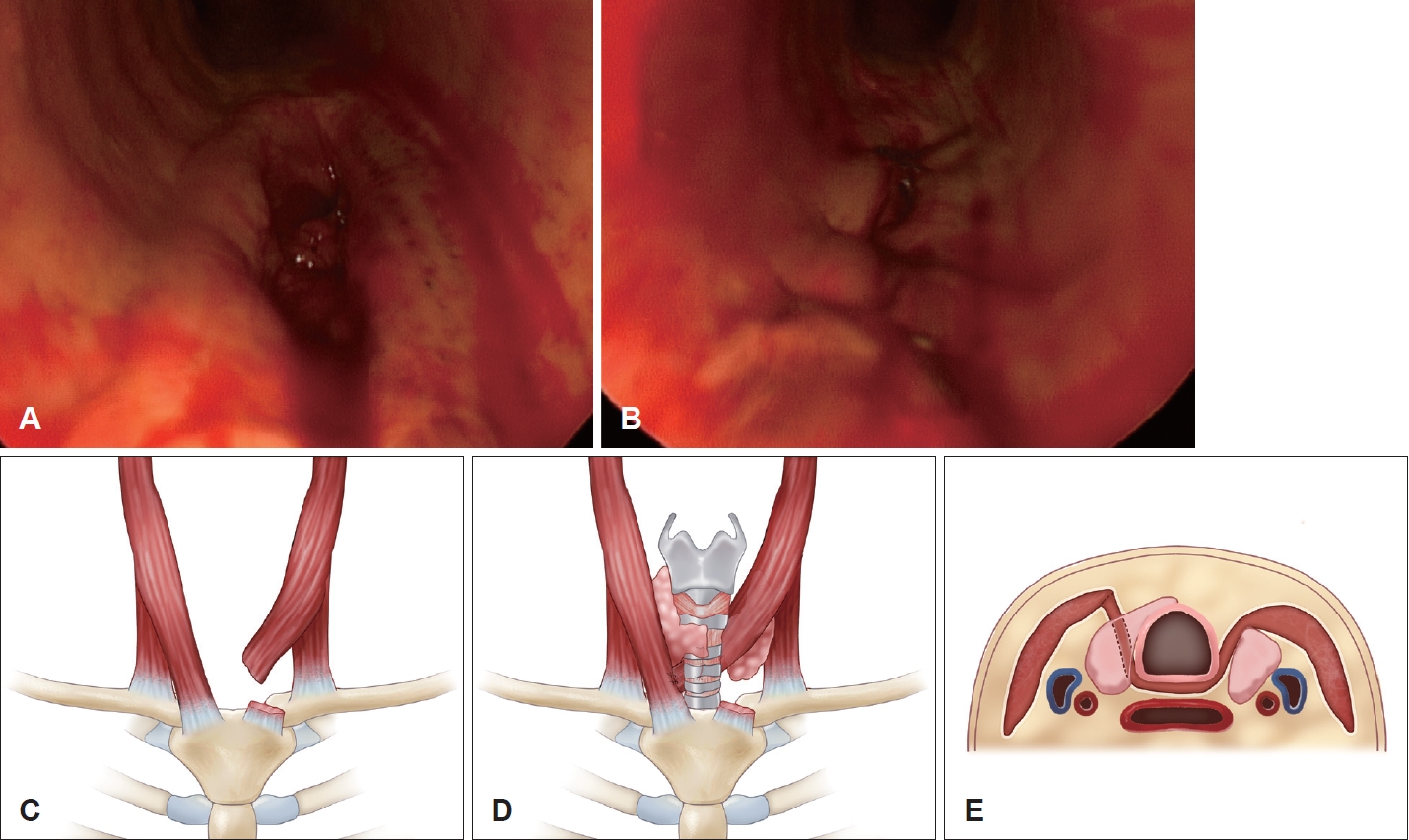
Fig. 4.Postoperative contrast-enhanced neck CT scan, 2 months after reinforcement. A: The mediastinal emphysema had disappeared. B: Soft tissue density (arrows) represents the transposed sternocleidomastoid muscle. C: An endoscopic exam revealed the presence of granulation with the posterior tracheal wall. 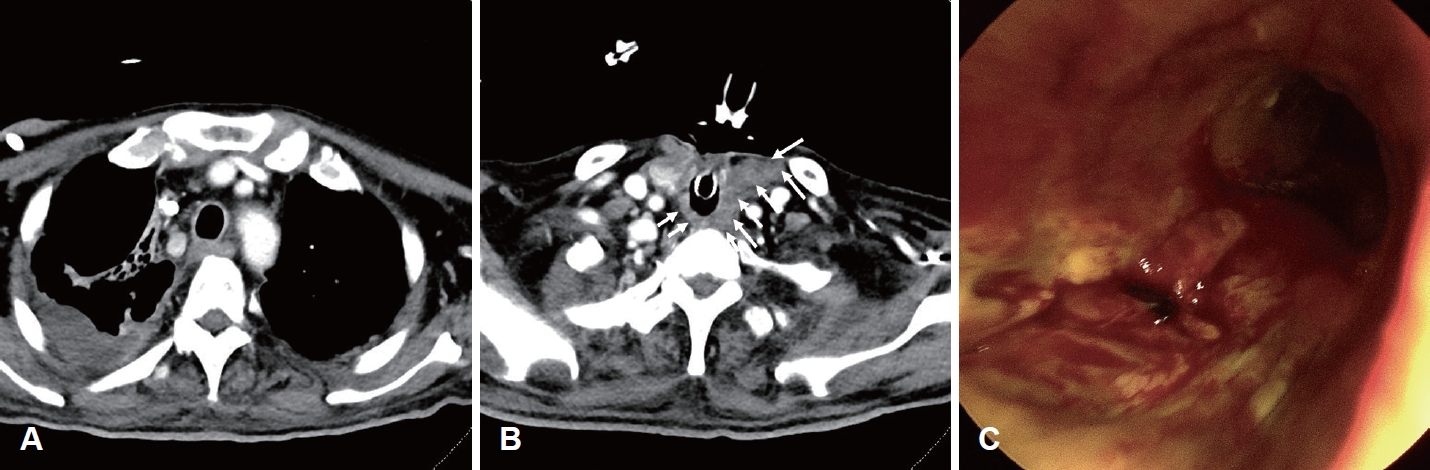
REFERENCES1. Jung YC, Sung K, Cho JH. Iatrogenic tracheal posterior wall perforation repaired with bronchoscope-guided knotless sutures through tracheostomy. Korean J Thorac Cardiovasc Surg 2018;51(4):277-9.
2. Deganello A, Sofra MC, Facciolo F, Spriano G. Tracheotomy-related posterior tracheal wall rupture, trans-tracheal repair. Acta Otorhinolaryngol Ital 2007;27(5):258-62.
3. Trottier SJ, Hazard PB, Sakabu SA, Levine JH, Troop BR, Thompson JA, et al. Posterior tracheal wall perforation during percutaneous dilational tracheostomy: an investigation into its mechanism and prevention. Chest 1999;115(5):1383-9.
4. Welter S, Krbek T, Halder R, Stamatis G. A new technique for complete intraluminal repair of iatrogenic posterior tracheal lacerations. Interact Cardiovasc Thorac Surg 2011;12(1):6-9.
5. Escott AB, Pochin RS. Repair of a posterior perforation of the trachea following thyroidectomy with a muscle transposition flap. Ear Nose Throat J 2016;95(2):E14-7.
6. Lee LM, Razi A. Three-layer technique to close a persistent tracheo-oesophageal fistula. Asian J Surg 2004;27(4):336-8.
7. Zhang X, Zhao R, Wang G, Chen Y, Ding P, Yang X, et al. Island sternocleidomastoid myocutaneous flap for posterior pharyngeal wall defect repair after anterior cervical spine surgery. Int Wound J 2022;19(1):169-77.
8. Friedman M, Toriumi DM, Owens R, Grybauskas VT. Experience with the sternocleidomastoid myoperiosteal flap for reconstruction of subglottic and tracheal defects: modification of technique and report of long-term results. Laryngoscope 1988;98(9):1003-11.
9. Han WH, Lee YI, Baek S, Seok J. [Tracheostomy performed by a head and neck surgeon under the supervision of an intensive care unit specialists in the COVID-19 era: a retrospective analysis]. J Korean Soc Laryngol Phoniatr Logop 2022;33(2):97-102, Korean.
10. Morris LL, Whitmer A, McIntosh E. Tracheostomy care and complications in the intensive care unit. Crit Care Nurse 2013;33(5):18-30.
12. Goldenberg D, Ari EG, Golz A, Danino J, Netzer A, Joachims HZ. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg 2000;123(4):495-500.
13. Foroulis CN, Nana C, Kleontas A, Tagarakis G, Karapanagiotidis GT, Zarogoulidis P, et al. Repair of post-intubation tracheoesophageal fistulae through the left pre-sternocleidomastoid approach: a recent case series of 13 patients. J Thorac Dis 2015;7(Suppl 1):S20-6.
|
|
|||||||||||||||||||||||||||||||||||||

 |
 |