 |
 |
AbstractBackground and Objectives Central compartment atopic disease (CCAD) has been studied with increasingly more importance as a distinct subtype of chronic rhinosinusitis with nasal polyp (CRSwNP). Studies have shown that CCAD in Western populations show a strong association with allergy and typical features of medial nasal structure and sinus involvement. The purpose of this study was to evaluate the clinical characteristics of CCAD and compare them to those of other subtypes of CRS in Korea.
Subjects and Method A chart review was performed retrospectively at two tertiary rhinologic centers for patients who were treated with bilateral endoscopic sinus surgery for CRS with or without nasal polyp from January 2019 to December 2021. Patients were divided into three groups, namely CCAD, CRSwNP, and CRS without nasal polyps (CRSsNP), and demographics, clinical characteristics, and imaging data were compared among the three groups.
Results A total of 150 patients were included in this study (50 patients in each group). CCAD showed similar nasal symptoms with CRSwNP, but higher rates of olfactory impairment than CRSsNP did. Allergy prevalence, serum total immunoglobulin E, and serum eosinophil were significantly higher in CCAD than in CRSwNP or CRSsNP. In CT scans of paranasal sinuses, CCAD showed significantly less haziness of maxillary sinus and higher ethmoid/maxillary score ratio than the other two groups. In addition, CT scans showed mucosal involvements of central compartment in CCAD.
Conclusion CCAD has characteristic endoscopic and imaging findings, showing a high prevalence of allergy and a strong association with the markers of type 2 inflammation. Therefore, CCAD is a distinct disease of CRSwNP and its allergic etiology should be considered in the management of patients with CCAD phenotype.
IntroductionChronic rhinosinusitis (CRS) is a complex inflammatory disease affecting the nose and paranasal sinuses (PNS), persisting 12 weeks or more. Classically, primary CRS has been separated into two major subtypes based upon phenotypic appearance; CRS with nasal polyps (CRSwNP) and CRS without nasal polyps (CRSsNP) [1]. Recently, central compartment atopic disease (CCAD) has been defined as a variant CRSwNP which involves inflammation or polypoid changes within the central structures of the nasal cavity including middle turbinate (MT), superior turbinate (ST) and the posterosuperior nasal septum (PSNS) [2,3]. White, et al. [4] first proposed the concept of the association between edema of MT and atopic disease. DelGaudio, et al. [2] reported that the atopic process involved not only the MT, but also other structures of central compartment in nasal cavity.
The clinical characteristics of CCAD and its association with allergy have been mainly studied, mostly led by Westerns. The radiologic pattern on CT of PNS demonstrates central nasal soft tissue thickening, with more significant disease progressing to secondary obstruction of the sinuses. A typical pattern is opacification of medial nasal cavity and sinuses, along with peripheral clearing along the lamina papyracea, ethmoid skull base, and lateral aspects of the maxillary sinuses. Hamizan, et al. [5] described that these central radiologic patterns on sinus PNS CT are associated with allergy status. An association between CCAD and allergy was further supported by additional studies in which almost all CCAD patients had a positive allergy status [2,3,6]. The rationale is that inhalant allergen deposit in the central compartment structures related to the course of normal nasal airflow and the allergy induced mucosal inflammation may lead to sinus ostial obstruction, and thus, secondary infection.
Although CCAD has been increasingly studied as a distinct subtype of CRS, there has been few reports on the study of CCAD in East Asia. Therefore, the objective of the present study was to determine the clinical and radiologic characteristics of CCAD compared to other phenotypes of CRS in Korea.
Subjects and MethodsStudy design and patientsWe performed a retrospective chart review on all patients who had been operated under the diagnosis of CRS on both sides at two tertiary academic centers from January 2019 to December 2021. Diagnosis of CRS was made based on national guidelines established by American Academy of Otolaryngology and European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS) [7,8]. Patients over 18 years old who underwent bilateral endoscopic sinus surgery under general anesthesia were included in the study, and exclusion criteria are as follows: tumorous condition (e.g. malignancy, inverted papilloma, vascular tumor), systemic immune disorder (Immunodeficiency, autoimmune disease), cystic fibrosis, Wegener’s or other autoimmune disease, revision surgery, or patients with incomplete data. This study was approved by the Institutional Research Board of our hospital and was conducted in compliance with the Declaration of Helsinki.
This study was approved by the Korea University Medical Center Institutional Review Board (2021GR0611).
MeasuresFor all enrolled patients, gender, age, smoking history, underlying disease, previous nasal operation history, allergy test results, asthma, serum total immunoglobulin E (IgE), serum eosinophil (percentages and counts), and initial nasal symptoms were reviewed.
Preoperative nasal endoscopic images were analyzed and used to classify the patients. Preoperative PNS CT scans were also reviewed to evaluate severity of sinusitis, ethmoid/maxillary score (E/M) ratio and mucosal involvement. The severity of sinusitis was evaluated with the Lund-Mackay (L-M) score and we checked the haziness for 6 sites (anterior ethmiod sinus, posterior ethmiod sinus, frontal sinus, sphenoid sinus, maxillary sinus and ostiomeatal complex) and then ranked from 0 to 2 (normal state: 0, partial hazziness: 1, total hazziness: 2) for each site. Using to the haziness scores of each sinus in L-M score, E/M ratio was calculated. We also determined whether mucosal involvement on CT scans was seen in the following four parts: MT, NS, nasal cavity, and olfactory cleft. Analysis of nasal endoscopy and PNS CT were conducted by two independent rhinologists.
Group classificationAll enrolled patients were classified into three study groups according to the initial nasal endoscopic findings; CCAD group, CRSwNP group and CRSsNP group. CCAD was diagnosed based on nasal endoscopic findings of inflammation or polypoid changes located within the central compartment (MT, PSNS, and/or ST). Patients with nasal polyps without these findings of CCAD were classified into the CRSwNP, and the remaining patients (no findings of CCAD or nasal polyps) were classified into CRSsNP. Patients whose nasal polyps were so large or many that the site of origin could not be identified by initial nasal endoscopic images, or whose central compartments could not be definitely evaluated due to structural problems were excluded. We also excluded the patients who met the diagnostic criteria for aspirin-exacerbated respiratory disease (AERD) or allergic fungal rhinosinusitis (AFRS), because these were discrete subtypes of CRSwNP and known to be a very small percentage for Asians.
A total of 50 patients were classified into the CCAD group according to the above diagnostic procedure. Age and gender matched samples were extracted from the CRSwNP and CRSsNP (50 patients in each group), and we compared the measure among the three groups.
Statistical analysesStatistical analyses were performed using IBM SPSS version 22.0 program (IBM Corp., Armonk, NY, USA). The numerical data were expressed as mean±standard deviation. One-way analyses of variance were performed followed by post-hoc test (Tukey, Duncan) for comparison of numerical data with normality between groups. Kruskal-Wallis test and Mann-Whitney U test were used to compare numerical data without normality between groups. For categorial data, the chi-square test and Fisher’s exact test were performed to compare groups. Statistical significance was set at p<0.05.
ResultsDemographic characteristics and nasal symptomsA total of 150 patients were included in this study (50 patients each in the CCAD, CRSwNP, and CRSsNP). Table 1 shows the demographic characteristics and initial nasal symptoms of patients. There were no significant differences in age, gender, smoking history and asthma among the three groups. As for the initial nasal symptoms, we determined whether the patients complained about the following 5 symptoms; nasal obstruction, rhinorrhea, sneezing, postnasal drip, and olfactory impairment. The most common nasal symptom was nasal obstruction in all study groups (90%, 86% and 74% respectively). Olfactory impairment was significantly more prevalent in the CCAD and CRSwNP than in the CRSsNP, and the other 4 nasal symptoms were not significantly different among three groups. Overall, CCAD and CRSwNP showed similar features of nasal symptoms.
Allergy prevalence and serologic resultsAllergy-sensitization was determined by either skin prick test or serologic assessment, in which serum allergen specific IgE greater than 0.35 kU/L was considered a positive result. The prevalence of allergy-sensitization was 90% in CCAD, 32% in CRSwNP, and 30% in CRSsNP respectively, which was significantly higher in CCAD than in the other two groups. In serologic test, all three results of total IgE (kU/L), eosinophil percentage (%) and eosinophil count (/μL) were significantly higher in CCAD than in CRSwNP or CRSsNP (Fig. 1).
Radiologic assessment
Table 2 shows L-M score and haziness for each site analyzed by PNS CT scans among three groups. L-M score was the highest in CRSwNP (15.84±4.77). followed by CCAD (12.26±4.43) and CRSsNP (9.42±4.45). CRSwNP showed the highest L-M score for all six sites among three groups. In CCAD, the score of maxillary sinuses was significantly lower than that of CRSwNP or CRSsNP. However, the score of ethmoid sinuses was not significantly different from CRSwNP and significantly higher than CRSsNP.
E/M ratio was calculated as using an algorithm ([sum of both anterior ethmoid sinuses+sum of both posterior ethmoid sinuses]/sum of both maxillary sinuses), and 6 cases with a summarized maxillary sinus score of 0 were converted to of 1 point. The E/M ratio in the CCAD group was significantly higher than in the other CRSwNP or CRSsNP (Fig. 2).
Mucosal involvement in PNS CT of the three groups was shown in Fig. 3. The CCAD showed a significantly higher rate of involvement than CRSwNP group in the MT and nasal septum on PNS CT scans. Compared with the CRSsNP, involvement of all 4 sites on CT scans were significantly higher in the CCAD.
DiscussionCCAD has recently been reported as a distinct phenotype of CRSwNP in various studies. White, et al. [4] first proposed polypoid change of the MT as an indicator of atopic disease, caused by inflammatory reaction between the allergens inhaled via nasal flow and the anterior aspects of MT. DelGaudio, et al. [2] revealed that other central nasal structures of ethmoid origin, including the posterior-superior nasal septum and the ST, are involved. If not treated in time, CCAD can lead to secondary involvement of the sinuses due to displacement of MT or extension of lateral polyposis of MT with medial-to-lateral progression.
Hamizan, et al. [5] described radiologic characteristics of CCAD. On PNS CT scans, there is a central focus of mucosal disease, and if the sinuses are involved, the roof or lateral wall tends to be relatively normal. They reported that these central radiologic patterns of mucosal disease are significantly associated with allergic etiology. Like this, previous studies have shown the unique clinical and radiological features of CCAD and its strong association with allergy. In EPOS 2020, CCAD was classified as a distinct disease in diffuse type 2 phenotype of primary CRS [8].
To the best of our knowledge, this study is the first report demonstrating the clinical and radiologic features of CCAD in Asia countries, compared to other phenotypes of CRS. The representative findings of three patients in this study are shown in Fig. 4. In a CCAD, nasal endoscope revealed polypoid change of MT and nasal septum. On PNS CT scan, the characteristic findings of total opacification in ethmoids and peripheral clearing in maxillary sinuses definitely observed. In the nasal endoscopic image of CRSwNP, multiple nasal polyps originating from the middle meatus were observed, and both ethmoids and maxillary sinuses had similar haziness on PNS CT scans. In CRSsNP, maxillary sinuses were more affected than ethmoids with no specific findings of nasal endoscopic images.
In the present study, we conducted a comparison of clinical and radiologic features among three groups, CCAD, CRSwNP, and CRSsNP, excluding AFRS and AERD. Although the specific prevalence of AFRS has not been reported, it is relatively low in East Asia compared to the West [9]. AERD is also a rare disease in East Asia, accounting for 0.57% of all CSR patients in China [10]. Therefore, we excluded AFRS and AERD because the significantly comparable number of the patients was not available, but instead included CRSsNP, which has not been included in previous studies as a comparison group of CRS patients.
The prevalence of allergy in CRS may vary by phenotype, with CCAD and AFRS having a stronger association than CRSwNP and CRSsNP [5,11]. In a previous study to analyze the allergy prevalence of each CRS phenotype, about 97.6% of CCAD patients were accompanied by allergy, showing the second highest association with allergy after AFRS (100%) [3]. Also in a study analyzing the clinical features of 15 CCAD patients, all 15 patients were allergy-sensitized [2].
In this study, although not as high as in previous studies, the allergy prevalence of CCAD patients was very high at 90%. Theoretically, all patients with CCAD would be expected to be allergy-sensitized because CCAD is a disease caused by allergic inhalants. The 5 cases of negative allergic result were thought to be due to local allergic rhinitis. We used the results of skin prick test and serologic test for allergy testing. However, there may be patients with local allergic rhinitis who have a localized allergic reaction in the nose without systemic atopy [12]. By combining the result of nasal provocation test as well as result of systemic atopy (skin test and serum-specific IgE test), the most comprehensive assessment of allergy prevalence would be obtained [13]. However, nasal provocation test were not available for this retrospective review and local allergic rhinitis was not evaluated.
The prevalence of asthma in CCAD was high compared to other groups, although not statistically significant. Since there have been studies showing a strong association between asthma and CRS with allergic rhinitis [14,15], it would be expected that there a relationship between CCAD and asthma. However, in previous Western studies, the prevalence of asthma was higher in patients with other subtypes of CRSwNP than in patients with CCAD [3,16]. Although CCAD is a disease induced by allergic inhalants, the relationship with asthma seems not yet clear. So further research is needed.
On the other hand, patients with CCAD showed significantly higher levels of serum total IgE and eosinophil (both percentage and count) than patients with other subtypes of CRS in this study. There have been many reports demonstrating a clinical significance of measuring total IgE in the evaluation and diagnosis of allergic rhinitis, and blood eosinophils are also known to be important markers of type 2 inflammation [17-19]. Considering that there are many cases of non-type 2 inflammation in CRSwNP in Asia and that almost all CCAD patients are positive for allergic rhinitis test, above results of this study were reasonable [20-22]. Although only children were included, there was also a study showing that patients with radiologic determined CCAD had higher serum total IgE levels compared to CRS patients without CCAD [23].
We classified patients with CRS into three groups based on nasal endoscopic findings, and compared findings of PNS CT scans. CCAD patients, endoscopic determined, had significantly less haziness of maxillary sinuses and high E/M ratio compared to other groups. Most of CCAD showed the representative findings, which sinus involvement starts in the medial parts of the ethmoid and maxillary sinuses with peripheral clearing, on CT scans.
CT scans showed the highest mucosal involvement of MT, nasal septum, olfactory cleft in CCAD. These results of CT scans have two important implications. First, CCAD in Asia also showed the imaging characteristics of CCAD patients in previous studies leaded mostly by the West. Second, nasal endoscopic determined CCAD reflect their representative features on CT, such as high E/M ratio, peripheral clearing of maxillary sinus, and mucosal involvement of central compartment. It could be supposed that the nasal endoscopic findings and PNS CT findings of CCAD are strongly associated.
Meanwhile, the nasal symptoms of CCAD were not significantly different from those of CRSwNP. Compared with CRSsNP, olfactory impairment were reported significantly more, which is a major symptom of CCAD. Olfactory dysfunction of CRS is multifactorial. Conductive disorder is caused by mechanical obstruction of odorant transmission due to mucosal edema and nasal polyps. Sensorineural disorder is induced by inflammatory infiltration of eosinophil and cytokines within the olfactory neuroepithelium [24-26]. In CCAD, mucosa of central component in nasal cavity was mainly affected in nasal endoscopy and PNS CT images. In addition, eosinophil infiltration is also thought to be severe in patients with CCAD, a disease of type 2 inflammation. It is likely to result in both conductive and sensorineural disorders in the olfactory bulb in CCAD.
There are some limitations of this study. First, we classified patients by nasal endoscopic imaging and selection bias may be induced by subjective opinion in this process. Second, other phenotypes of CRSwNP, such as AERD and AFRS, were not included in this study due to low prevalence in East Asia. Finally, our retrospective data does not contain the information of prognosis including recurrence, revision surgery, and postoperative management. Therefore, a study on the prognosis and management of CCAD is needed in the future, including other phenotypes of CRSwNP.
In conclusion, CCAD is a distinct phenotype of CRSwNP showing characteristic nasal endoscopic and imaging findings with a high prevalence of allergy and olfactory impairment.
NotesAuthor Contribution Conceptualization: Heung-Man Lee. Data curation: Heung-Man Lee, Jae Hoon Cho, Yong-Dae Kim. Formal analysis: Su-Jong Kim, Hwaejoon Jung, Jee Won Moon. Investigation: Hwaejoon Jung, Jee Won Moon. Methodology: Heung-Man Lee, Jae Hoon Cho, Yong- Dae Kim. Supervision: Heung-Man Lee. Validation: Heung-Man Lee, Jae Hoon Cho, Yong-Dae Kim. Writing—original draft: Hwaejoon Jung, Su-Jong Kim, Jee Won Moon. Writing—review & editing: Jee Won Moon, Heung-Man Lee. Fig. 1.Prevalence of allergy-sensitization and results of serologic tests in the three groups. A: Allergen-sensitization. B: Serum total immunoglobulin E level. C: Serum eosinophil percentage. D: Serum eosinophil count. *p<0.05. CCAD, central compartment atopic disease; CRSwNP, chronic rhinosinusitis with nasal polyp; CRSsNP, chronic rhinosinusitis without nasal polyp. 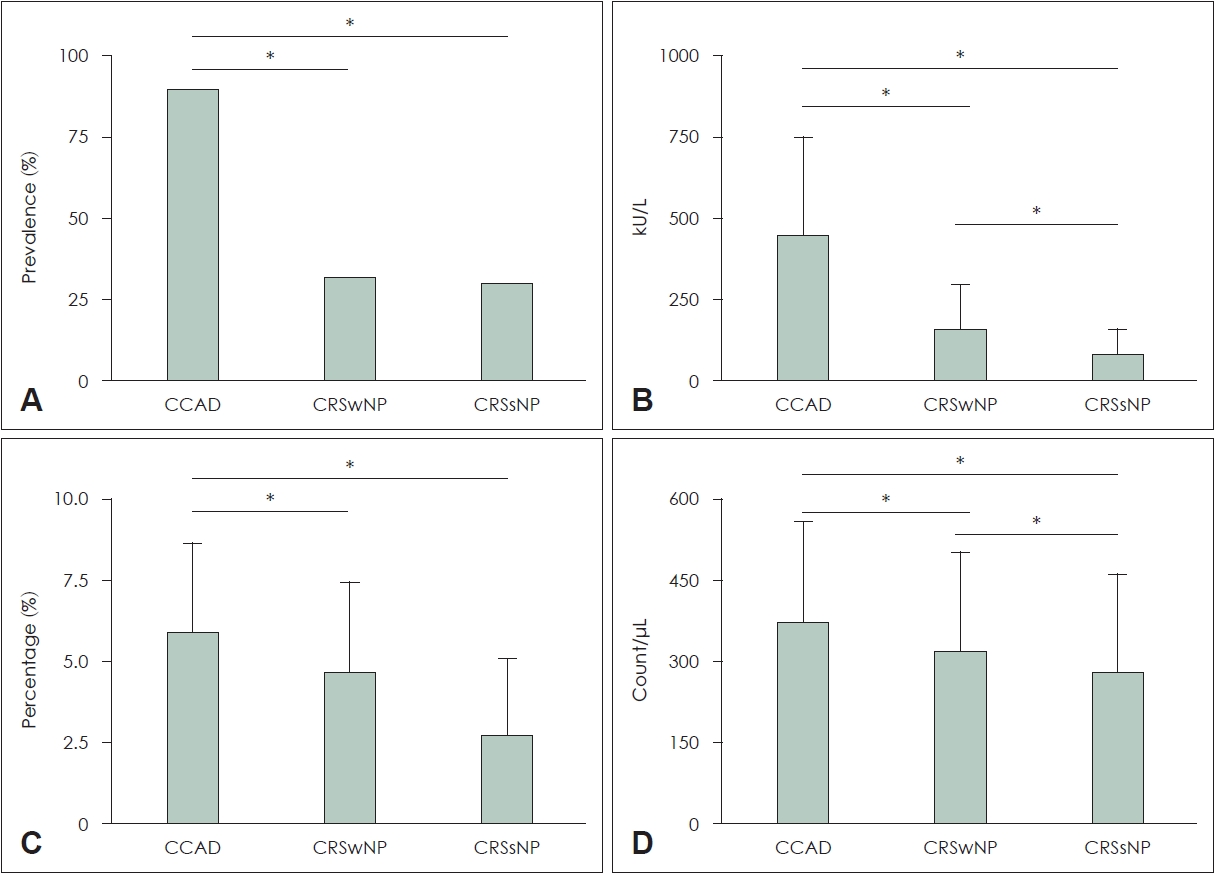
Fig. 2.E/M ratio in the three groups. *p<0.05. E/M, ethmoid/maxillary score; CCAD, central compartment atopic disease; CRSwNP, chronic rhinosinusitis with nasal polyp; CRSsNP, chronic rhinosinusitis without nasal polyp. 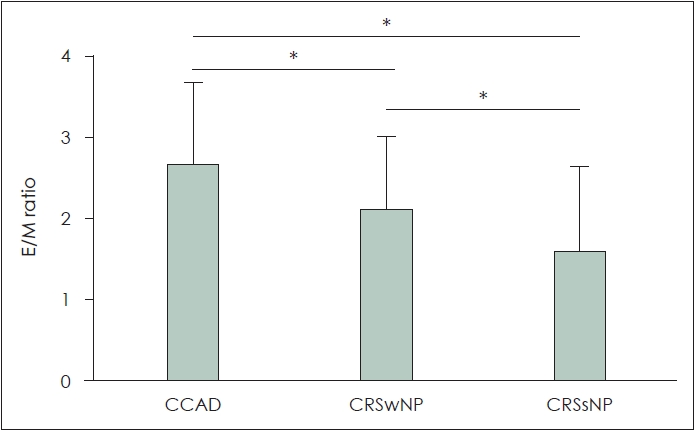
Fig. 3.Mucosal involvement on paranasal sinuses CT scans for the following 4 sites. A: Middle turbinate. B: Nasal septum. C: Nasal cavity. D: Olfactory cleft. *p<0.05. CCAD, central compartment atopic disease; CRSwNP, chronic rhinosinusitis with nasal polyp; CRSs- NP, chronic rhinosinusitis without nasal polyp. 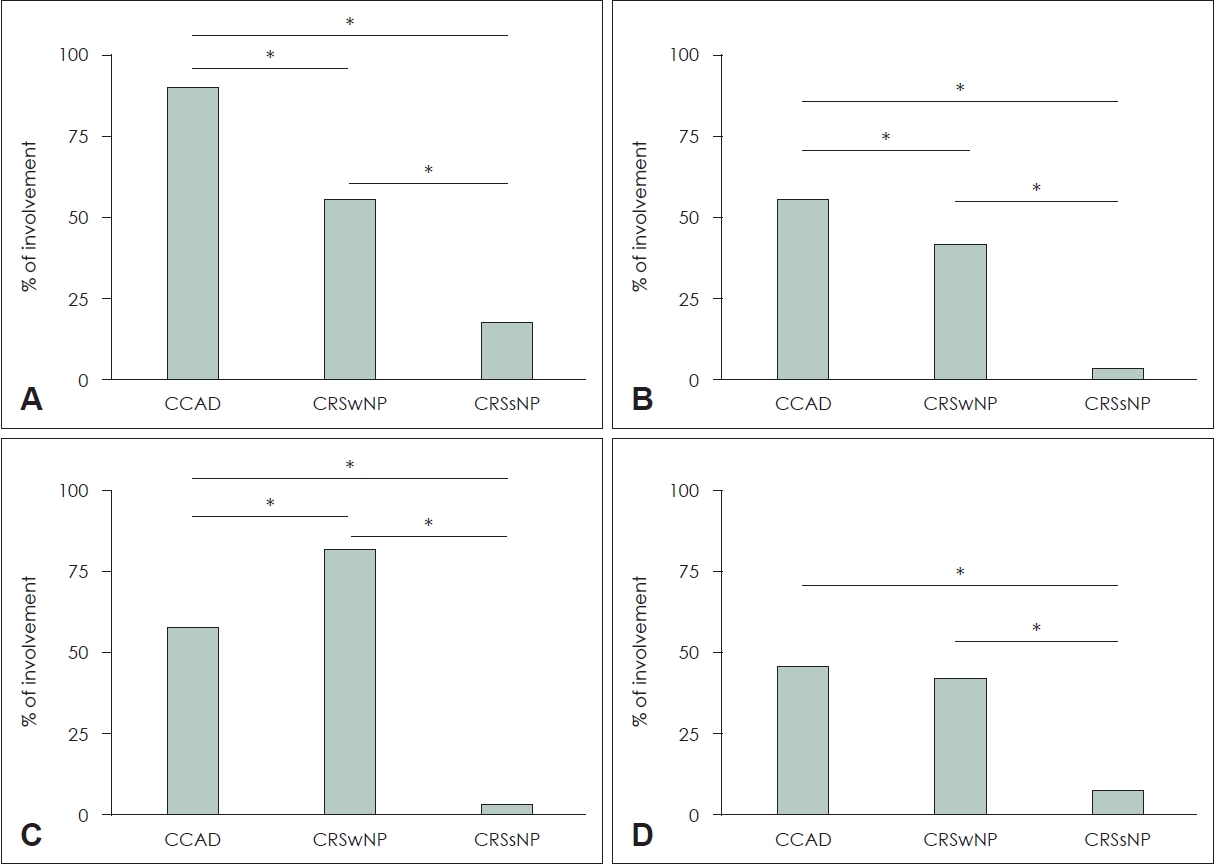
Fig. 4.Representative nasal endoscopic and radiologic features of three groups: CCAD (A and D), CRSwNP (B and E), and CRSsNP (C and F). CCAD, central compartment atopic disease; CRSwNP, chronic rhinosinusitis with nasal polyp; CRSsNP, chronic rhinosinusitis without nasal polyp; S, nasal septum; M, middle turbinate. 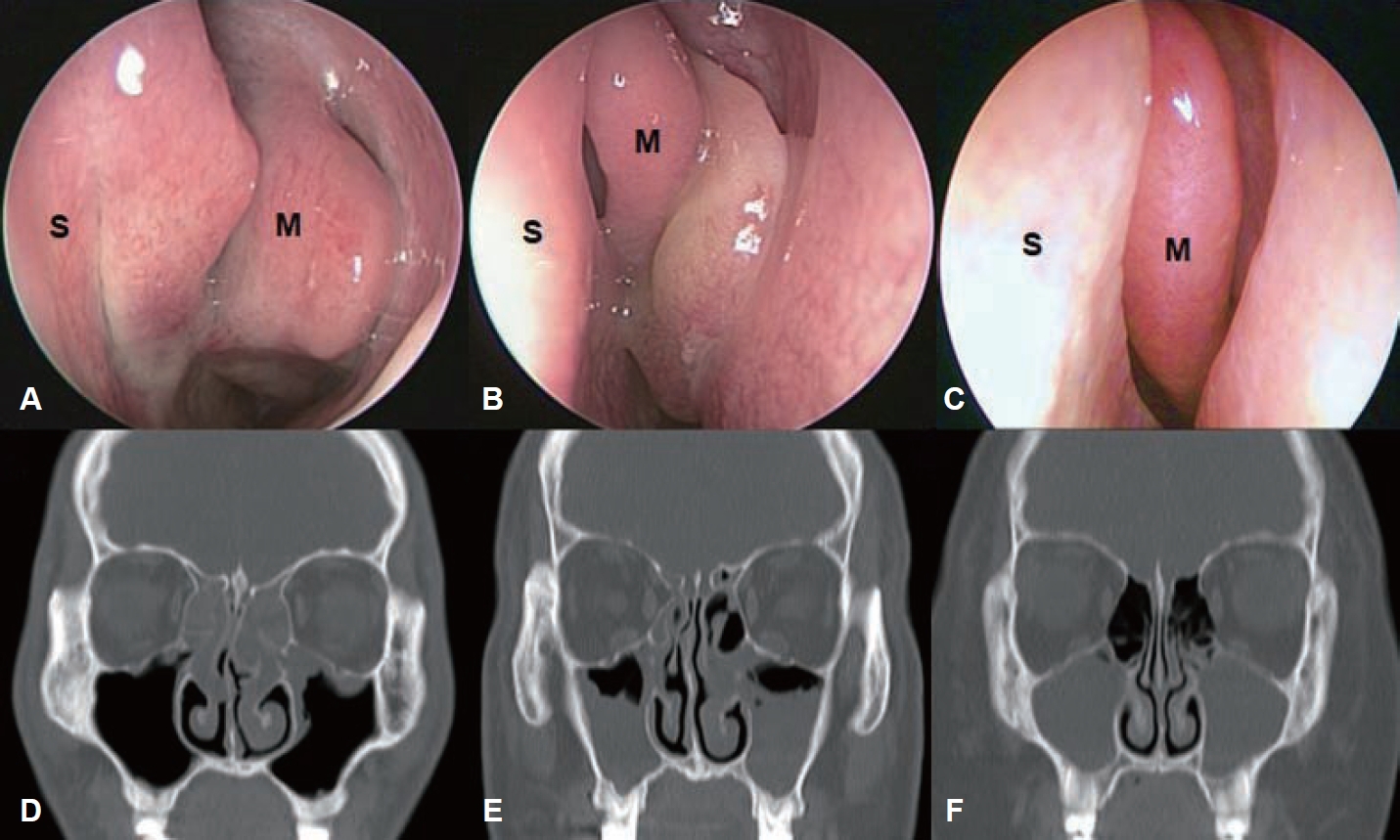
Table 1.Demographic characteristics and nasal symptoms of the three groups
*CCAD and CRSwNP showed significantly higher rates of olfactory impairment than CRSsNP, and there was no significant difference between CCAD and CRSwNP. CCAD, central compartment atopic disease; CRSwNP, chronic rhinosinusitis with nasal polyp; CRSsNP, chronic rhinosinusitis without nasal polyp; ns, not significant Table 2.Comparison of imaging findings on PNS CT scans among the three groups Pair wise comparison of three groups was performed using the Mann-Whitney U test: p1, CCAD vs. CRSwNP; p2, CCAD vs. CRSsNP; p3, CRSwNP vs. CRSsNP. PNS, paranasal sinuses; CCAD, central compartment atopic disease; CRSwNP, chronic rhinosinusitis with nasal polyp; CRSsNP, chronic rhinosinusitis without nasal polyp; ns, not significant REFERENCES1. Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 2012;50(1):1-12.
2. DelGaudio JM, Loftus PA, Hamizan AW, Harvey RJ, Wise SK. Central compartment atopic disease. Am J Rhinol Allergy 2017;31(4):228-34.
3. Marcus S, Schertzer J, Roland LT, Wise SK, Levy JM, DelGaudio JM. Central compartment atopic disease: Prevalence of allergy and asthma compared with other subtypes of chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol 2020;10(2):183-9.
4. White LJ, Rotella MR, DelGaudio JM. Polypoid changes of the middle turbinate as an indicator of atopic disease. Int Forum Allergy Rhinol 2014;4(5):376-80.
5. Hamizan AW, Loftus PA, Alvarado R, Ho J, Kalish L, Sacks R, et al. Allergic phenotype of chronic rhinosinusitis based on radiologic pattern of disease. Laryngoscope 2018;128(9):2015-21.
6. Brunner JP, Jawad BA, McCoul ED. Polypoid change of the middle turbinate and paranasal sinus polyposis are distinct entities. Otolaryngol Head Neck Surg 2017;157(3):519-23.
7. Rosenfeld RM, Andes D, Bhattacharyya N, Cheung D, Eisenberg S, Ganiats TG, et al. Clinical practice guideline: Adult sinusitis. Otolaryngol Head Neck Surg 2007;137(Suppl 3):S1-31.
8. Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 2020;58(Suppl S29):1-464.
9. Lee SH, Kim HJ, Lee JW, Yoon YH, Kim YM, Rha KS. Categorization and clinicopathological features of chronic rhinosinusitis with eosinophilic mucin in a Korean population. Clin Exp Otorhinolaryngol 2015;8(1):39-45.
10. Fan Y, Feng S, Xia W, Qu L, Li X, Chen S, et al. Aspirinexacerbated respiratory disease in China: A cohort investigation and literature review. Am J Rhinol Allergy 2012;26(1):e20-2.
11. Philpott CM, Erskine S, Hopkins C, Kumar N, Anari S, Kara N, et al. Prevalence of asthma, aspirin sensitivity and allergy in chronic rhinosinusitis: Data from the UK national chronic rhinosinusitis epidemiology study. Respir Res 2018;19(1):129.
12. Rondón C, Campo P, Togias A, Fokkens WJ, Durham SR, Powe DG, et al. Local allergic rhinitis: Concept, pathophysiology, and management. J Allergy Clin Immunol 2012;129(6):1460-7.
13. Augé J, Vent J, Agache I, Airaksinen L, Campo Mozo P, Chaker A, et al. EAACI position paper on the standardization of nasal allergen challenges. Allergy 2018;73(8):1597-608.
14. Bachert C, Van Bruaene N, Toskala E, Zhang N, Olze H, Scadding G, et al. Important research questions in allergy and related diseases: 3-chronic rhinosinusitis and nasal polyposis - a GALEN study. Allergy 2009;64(4):520-33.
15. Feng CH, Miller MD, Simon RA. The united allergic airway: Connections between allergic rhinitis, asthma, and chronic sinusitis. Am J Rhinol Allergy 2012;26(3):187-90.
16. DelGaudio JM. Central compartment atopic disease: The missing link in the allergy and chronic rhinosinusitis with nasal polyps saga. Int Forum Allergy Rhinol 2020;10(10):1191-2.
17. Kalpaklioglu AF, Kavut AB. Allergic and nonallergic rhinitis: Can we find the differences/similarities between the two pictures? J Asthma 2009;46(5):481-5.
18. Min HJ, Hong YH, Yang HS, Kim KS. The correlation of serum eosinophil cationic protein level with eosinophil count, and total IgE level in Korean adult allergic rhinitis patients. Asian Pac J Allergy Immunol 2016;34(1):33-7.
19. Jung YG, Kim KH, Kim HY, Dhong HJ, Chung SK. Predictive capabilities of serum eosinophil cationic protein, percentage of eosinophils and total immunoglobulin E in allergic rhinitis without bronchial asthma. J Int Med Res 2011;39(6):2209-16.
20. Kim DW. Can neutrophils be a cellular biomarker in Asian chronic rhinosinusitis? Clin Exp Otorhinolaryngol 2019;12(4):325-6.
21. Mahdavinia M, Suh LA, Carter RG, Stevens WW, Norton JE, Kato A, et al. Increased noneosinophilic nasal polyps in chronic rhinosinusitis in US second-generation Asians suggest genetic regulation of eosinophilia. J Allergy Clin Immunol 2015;135(2):576-9.
22. Yang JH, Kim DK. New discoveries regarding endotypes of chronic rhinosinusitis with nasal polyp. Korean J Otorhinolaryngol-Head Neck Surg 2017;60(9):431-6.
23. Lee K, Kim TH, Lee SH, Kang CH, Je BK, Oh S. Predictive value of radiologic central compartment atopic disease for identifying allergy and asthma in pediatric patients. Ear Nose Throat J 2022;101(9):593-9.
24. Lane AP, Turner J, May L, Reed R. A genetic model of chronic rhinosinusitis-associated olfactory inflammation reveals reversible functional impairment and dramatic neuroepithelial reorganization. J Neurosci 2010;30(6):2324-9.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |