 |
 |
AbstractBackground and Objectives Sufficient training is essential before starting rhinoplasty due to the nature of the surgery, and how to effectively teach rhinoplasty is a major issue in otolaryngology education. The Korean Academy of Facial Plastic and Reconstruction Surgery conducts an annual rhinoplasty hands-on course using a silicone model. The aim of this study was to evaluate the effectiveness of the course using a dummy nose model in rhinoplasty education.
Subjects and Method The annual rhinoplasty hands-on course for beginners was conducted as a dry laboratory surgical simulation equipped with adequate surgical instruments for rhinoplasty. A commercialized silicone nose model for rhinoplasty was provided to each of the 15 trainees and instructors. A 5-point Likert scale questionnaire was given before and after the course.
Results The 15 trainees, consisted of 9 otorhinolaryngology specialists, 5 residents, and 1 private physician. Of the responses, 92.8% were positive about the similarity between the dummy and real human tissue. A step-by-step evaluation was conducted: trainees and instructors were most satisfied with osteotomy, giving it the highest score. After the course, the trainees responded that their knowledge and skills in rhinoplasty improved. Of the trainees, 86.6% answered that they were either strongly or very strongly confident about the rhinoplasty procedure. Instructors evaluated the courses as suitable for rhinoplasty education.
IntroductionProficiency in rhinoplasty requires an extensive training combined with a long learning curve. According to the study in the United States, only 18% of mid-year postgraduate year-5 residents reported that they had independently performed rhinoplasty [1]. Given the inherent nature of rhinoplasty, inadequate training among physicians can lead to unfavorable outcomes, encompassing both cosmetic and functional aspects. Therefore, sufficient training is essential before starting rhinoplasty, and how to effectively teach rhinoplasty is a major issue in otolaryngology education. Repeated practice under supervision during surgery consists traditional apprenticeship model of surgical education, but the quality of the training can be limited by highly complex procedures [2]. Therefore, useful, cost-effective, and reliable learning models are needed, and animal models, cadaveric dissection procedures, virtual learning, and 3-dimensional (3D) silicone simulators have been raised as possible candidates [3,4]. Among them, 3D silicone simulators for surgery are widely used in other surgical fields such as maxillary sinus lift, congenital heart disease, and strabismus [5-7]. However, there is limited supporting evidence regarding the effectiveness of 3D silicone simulators in the field of rhinoplasty education. This study aimed to assess the effect of utilizing 3D silicone simulators as an educational tool for novice participants in rhinoplasty during a rhinoplasty hands-on course organized by the Korean Academy of Facial Plastic and Reconstructive Surgery (KAFPRS) [8].
Materials and MethodsSurgical simulatorThe surgical 3D simulator for rhinoplasty (Simulare Medical Corp., Ontario, Canada) made of silicone was used in the rhinoplasty hands-on course (Fig. 1). The 3D silicone simulator allows trainees to practice major steps of rhinoplasty including incision, flap elevation, osteotomy, septoplasty, tip surgery, and dorsal augmentation [8]. There are detailed types of simulators including deviated nose, crooked nose, posttraumatic nose, and Asian bulbous nose with dorsal hump models available. For this study, the hump nose type of the simulator was used in the training course.
SurveysThe rhinoplasty hands-on course was held at a medical dry lab, and 15 each trainees and instructors participated. Questionnaires were given to both trainees and instructors, 2-parts to the trainees and 1-part to the instructors. The first part of the survey given to the participants before the course included previous experience in rhinoplasty, expectations for the course, and confidence in rhinoplasty procedures. During the post-course survey’s second phase, the trainees were requested to assess the 3D model’s attributes, including its resemblance to an actual nose, as well as the usefulness of each step-by-step procedures. Additionally, the participants’ future intention to perform rhinoplasty and possible points to be improved were asked. Instructors were asked to evaluate the course in terms of teaching anatomy, surgical planning, and surgical skills and overall suitability of the course for rhinoplasty education after the course. Likert scale was used, and responses were kept anonymous. Also, the possible improvements of the course was asked to both trainees and instructors after the course, and answer choices include the model’s similarity to the real tissue, allocation of practice time, course fee paid by trainees, and training equipment.
ResultsParticipantsA total of 15 trainees, including 9 otorhinolaryngology specialists, 5 residents, and 1 private physician, and 15 teaching hospital faculties as instructors participated in the course. Although 14 of the trainees answered that they had experience assisting rhinoplasty, only 3 had independently performed rhinoplasty, which were 93.3% and 20.0%, respectively. About half of the trainees, 53.3%, reported that they had received training in rhinoplasty techniques before the course.
Resemblance to the human tissueOf the trainees, 71.4% indicated that the model exhibited moderate similarity to real human tissue, and 21.4% reported that the model displayed a high level of similarity. The bony part of the model was evaluated to have similar hardness to the real human tissue, compared to the skin and cartilaginous parts (Fig. 2). Tactile sensation was identified as the most distinct point from real human tissue by eight respondents (Table 1).
Step-by-step evaluationThe evaluation of each step in the rhinoplasty course (Fig. 3) was asked to both trainees and instructors (Fig. 4). Trainees and instructors were requested to answer whether the rhinoplasty hands-on course was helpful for learning each step of skin incision, flap elevation, osteotomy, tip plasty, and dorsal augmentation. Most of the trainees and instructors were satisfied with osteotomy, with highest score among procedures. Relatively, dorsal augmentation and skin incision were rated as relatively less satisfactory steps with the model.
Improvement of skills and confidenceTrainees’ expectations for the course were very high even before the course, and after the course, the impression has shifted to even more positive side. About 46.7% have answered that they were positive that the workshop would improve their rhinoplasty skills before the course, and 53.3% have answered that they were very positive. After the training course, 66.7% have answered that they were very positive that their knowledge and skills improved through the practice, and 33.3% have answered positive (Fig. 5).
The trainees were asked to report their confidence in rhinoplasty in the 5-point Likert scale. Sixty percent of the trainees showed weak or very weak confidence before the course, however, the trainees’ sense of competence has significantly increased after the course (pre: 2.5±1.2, post: 3.9±0.5, p=0.003) (Fig. 6).
Suitability for educationInstructors have evaluated the rhinoplasty hands-on course as very suitable for the rhinoplasty education. Fourty percent of the instructors were very positive about the hands-on course, in terms of teaching anatomy, surgical planning, and surgical skills, and 60% of the instructors answered they were positive. Also, 40% of the instructors have answered that the course’s model is appropriate for teaching rhinoplasty in general, and 60% were very positive about the overall educational suitability of the course.
Points to improveAfter the course, both trainees and instructors were asked about potential improvements. Four trainees expressed the need for improvement in the similarity of the model to real human tissue, while three trainees reported challenges in aligning their practice finishing time. Two trainees each answered course fee and training equipment can be improved. Additionally, five instructors suggested that the course fee paid by trainees should be adjusted.
DiscussionThe rhinoplasty hands-on course provided by the KAFPRS allows trainees to practice the major steps of rhinoplasty. The utilization of 3D silicone models, exhibiting anatomical similarity to human tissue, holds promising potential in surgical education for enhancing surgical outcomes in a safe and efficient manner [9]. The commercially developed surgical simulator for rhinoplasty (Simulare Medical Corp.) used in this study enables a practical, step-by-step, and end-to-end approach to rhinoplasty. The strengths of the model are described as multi-layered, including skin, subcutaneous tissue, and perichondrium with complete nasal anatomy and anatomical planes, including nasal septum, upper lateral, lower lateral, and accessory cartilages.
In this study, prior to the course, the majority of participants reported having experience in assisting with rhinoplasty, while only a minority had independently conducted rhinoplasty procedures by themselves. In the otorhinolaryngology field, 3D silicone simulators are already utilized in some surgical training, including endoscopic sinus surgery to avoid potential risks in surgical training due to the lack of experience [10]. However, to guarantee not only the safety, but also accessibility and reliability of the education, evaluation of the model is essential.
In this study, trainees reported that the model generally resembled the human body. Participants were asked to evaluate the strength of the surgical simulator compared to human tissue for skin, cartilage, and bone, respectively. Bony part of the model was rated as relatively more similar the real human tissue compared to the cartilaginous and skin parts, probably due to the lower elasticity of silicone compared to real human tissue. However, flap elevation and layer-by-layer dissection were possible using the course’s model, which was an advantage for rhinoplasty beginners.
Moreover, trainees and instructors were asked whether the hands-on course was helpful for learning each step of skin incision, flap elevation, osteotomy, tip plasty, and dorsal augmentation, and most of them were satisfied with the training of osteotomy using the model, which might be due to the relatively higher resemblance of bony structure to the real tissue. In addition, according to the study in the United States that investigated otolaryngology residents before and after the hands-on course using surgical simulators, the residents reported to have the least knowledge with respect to osteotomy and tip plasty before the course [11]. Therefore, a 3D surgical simulator can be a feasible tool for rhinoplasty beginners to acquire osteotomy and tip plasty skills outside the operating room. Silicone, which was used in the course’s model is popular material for surgical simulators due to the availability and elasticity [12], but for more efficient training, continuous exploration of improvements for the model would be required.
The trainees became significantly more confident in rhinoplasty after the course, and instructors evaluated the hands-on course as suitable for rhinoplasty education. Also, instructors composed of attending physicians of teaching hospitals rated the hands-on course as appropriate for teaching rhinoplasty in terms of teaching anatomy, surgical planning and surgical techniques. As most trainees and instructors expressed that they were positive about the 3D model’s impact on education, the 3D models can become an important part of rhinoplasty education. Three-dimensional rhinoplasty simulators were reported to improve junior (PGY1-3) and senior (PGY4-5) residents’ knowledge regarding anatomies and surgical skills in the United States [11]. On the other hand, surgical training using simulators allows instructors to evaluate trainees’ technical performance efficiently outside the operating room [13].
For studies regarding education, selecting appropriately representative measurement of outcome is a challenge [13]. There are certain limitations of this study including small sample size. This study involved responses from a relatively small group of Otorhinolaryngology surgeons who attended the hands-on rhinoplasty course. The surgical simulator used in this study, the hump nose model, is just one of many clinical models. In addition, Likert scale questionnaires have the risk of response bias.
Rhinoplasty surgeons always needs to be technically proficient, but it becomes more difficult for Otorhinolaryngology residents to acquire these skills in the operating room due to the complexity of procedures. Although there are limitations to be improved, the hands-on course provided by the KAFPRS is evaluated as effective the education for beginners in rhinoplasty and would benefit their future surgical practice. Through the hands-on course, trainees can acquire knowledge and skills to make active and challenging attitudes about rhinoplasty and surgical decisions. Further studies including direct 3D model production and evaluation are considered to have both clinical and educational significance in the field of Rhinoplasty and Otorhinolaryngology.
In conclusion, the hands-on course for provided by the KAFPRS using silicone model similar to human tissue allows trainees to practice rhinoplasty techniques in a relatively safe and clean way. A 3D simulator can be a useful surgical training tool for rhinoplasty beginners.
ACKNOWLEDGMENTSThe authors thank all the instructors and participants in the rhinoplasty hands-on course at the Annual Congress of the Korean Academy of Facial Plastic and Reconstructive Surgery 2022.
NotesAuthor Contribution Conceptualization: Tae-Bin Won, Soo Whan Kim. Data curation: Minju Kim, Seung-No Hong, KAFPRS, Soo Whan Kim, Tae-Bin Won. Formal analysis: Minju Kim, Seung-No Hong, KAFPRS, Soo Whan Kim, Tae-Bin Won. Investigation: Minju Kim, Seung-No Hong, KAFPRS, Soo Whan Kim, Tae-Bin Won. Methodology: Minju Kim, Seung-No Hong, KAFPRS, Soo Whan Kim, Tae-Bin Won. Supervision: Soo Whan Kim, Tae-Bin Won. Visualization: all authors. Writing‚Äîoriginal draft: Minju Kim, Seung-No Hong, Soo Whan Kim, Tae-Bin Won. Writing‚Äîreview & editing: Minju Kim, Seung-No Hong, Soo Whan Kim, Tae-Bin Won. Fig.¬Ý1.The surgical simulator for rhinoplasty (Simulare Medical Corp.). A: Lateral view. B: Frontal view. 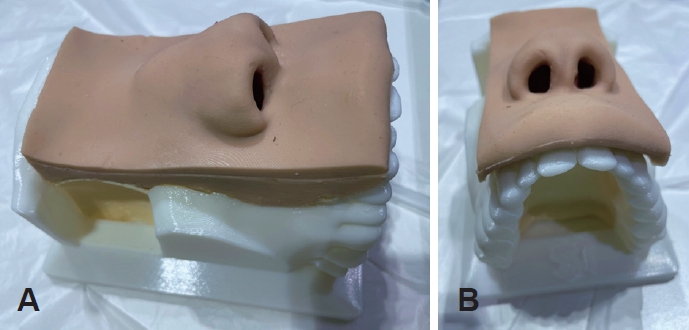
Fig.¬Ý2.The survey of model‚Äôs resemblance to the real human tissue. A: Resemblance of bony/cartilaginous/skin parts. B: Overall resemblance. 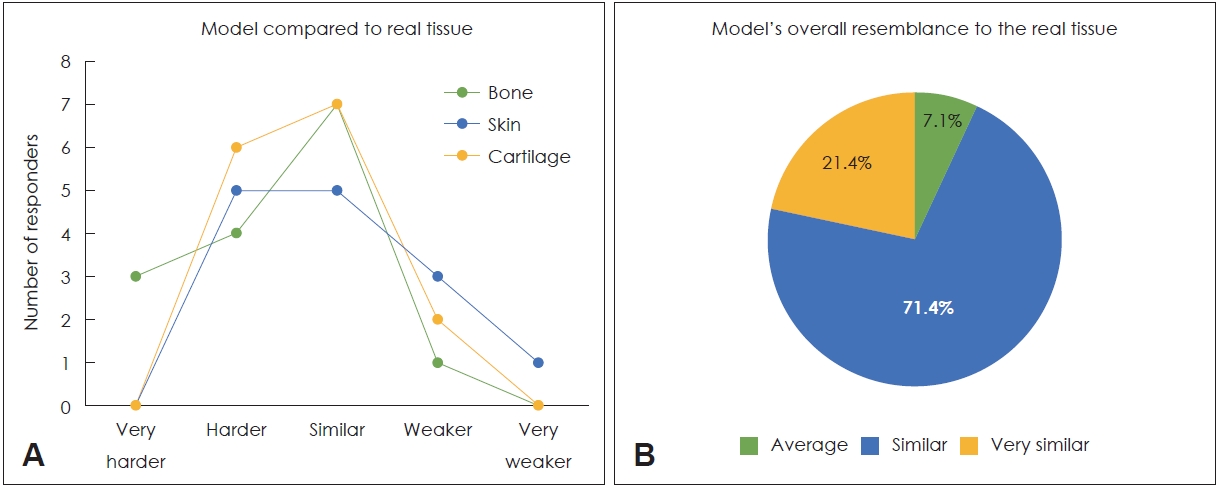
Fig.¬Ý3.Each step of rhinoplasty (A, skin incision; B, flap elevation; C, osteotomy; D, tip plasty; E, dorsal augmentation). 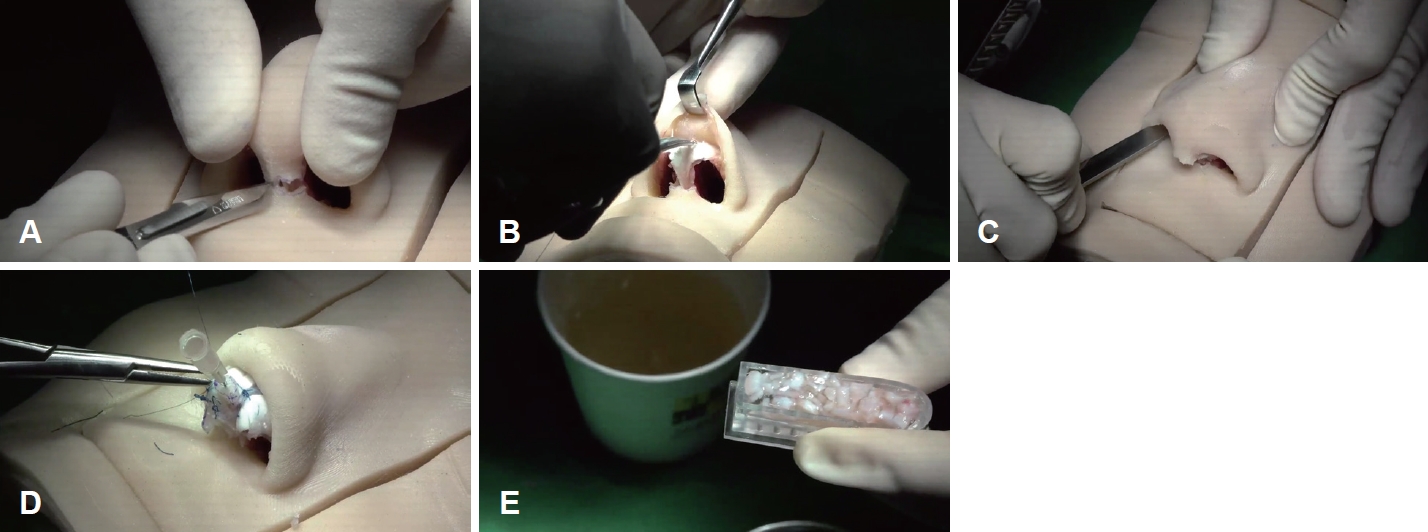
Fig.¬Ý4.Step-by-step evaluation of the course by trainees and instructors (*points: answers for each procedure [1: very unhelpful, 2: unhelpful, 3: neutral, 4: helpful, 5: very helpful] multiplied by 20). 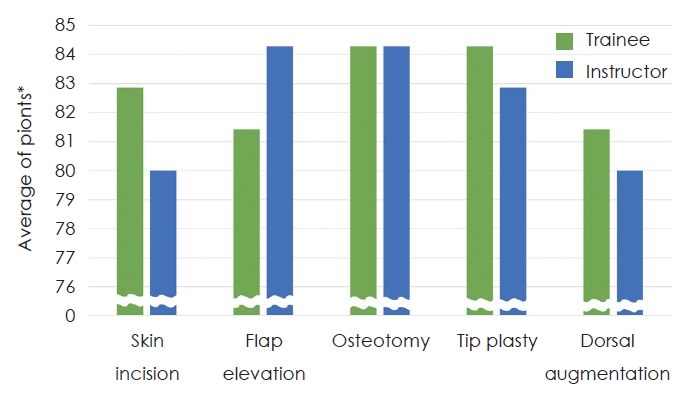
REFERENCES1. O’Brien DC, Kellermeyer B, Chung J, Carr MM. Experience with key indicator cases among otolaryngology residents. Laryngoscope Investig Otolaryngol 2019;4(4):387-92.
2. Steehler MK, Chu EE, Na H, Pfisterer MJ, Hesham HN, Malekzadeh S. Teaching and assessing endoscopic sinus surgery skills on a validated low-cost task trainer. Laryngoscope 2013;123(4):841-4.
3. Loh CYY, Wang AYL, Tiong VTY, Athanassopoulos T, Loh M, Lim P, et al. Animal models in plastic and reconstructive surgery simulation-a review. J Surg Res 2018;221:232-45.
4. McIntosh C, Patel KR, Lekakis G, Wong BJF. Emerging trends in rhinoplasty education: accelerated adoption of digital tools and virtual learning platforms. Curr Opin Otolaryngol Head Neck Surg 2022;30(4):226-9.
5. Werz SM, Zeichner SJ, Berg BI, Zeilhofer HF, Thieringer F. 3D printed surgical simulation models as educational tool by maxillofacial surgeons. Eur J Dent Educ 2018;22(3):e500-5.
6. Yoo SJ, Hussein N, Peel B, Coles J, van Arsdell GS, Honjo O, et al. 3D modeling and printing in congenital heart surgery: entering the stage of maturation. Front Pediatr 2021;9:621672.
7. Jagan L, Turk W, Petropolis C, Egan R, Cofie N, Wright KW, et al. Validation of a novel strabismus surgery 3D-printed silicone eye model for simulation training. J AAPOS 2020;24(1):3.e1-6.
8. Lee KI, Won TB, Hyun S, Song H, Jang YJ, Choi JY, et al. Dissection manual for open rhinoseptoplasty in a silicone nose model. J Rhinol 2022;29(1):1-12.
9. Zammit D, Safran T, Ponnudurai N, Jaberi M, Chen L, Noel G, et al. Step-specific simulation: the utility of 3D printing for the fabrication of a low-cost, learning needs-based rhinoplasty simulator. Aesthet Surg J 2020;40(6):NP340-5.
10. Chang DR, Lin RP, Bowe S, Bunegin L, Weitzel EK, McMains KC, et al. Fabrication and validation of a low-cost, medium-fidelity silicone injection molded endoscopic sinus surgery simulation model. Laryngoscope 2017;127(4):781-6.
11. Gupta N, Fitzgerald CM, Ahmed MT, Tohidi S, Winkler M. Feasibility of a 3D printed nasal model for resident teaching in rhinoplasty. J Plast Reconstr Aesthet Surg 2021;74(10):2776-820.
|
|
||||||||||||||||||||||||||||||||||||||||||

 |
 |