 |
 |
AbstractIn frontal sinus surgery, stenosis of the frontal sinus opening after surgery remains a challenge for many surgeons. Different surgical approaches such as Lynch procedure, Draf type II, and extended modified Lothrop procedure may decrease adverse surgical results but also accompany inherent complications. The use of various kinds of stents have been also suggested to prolong the patency of the frontal sinus opening. However, no definite consensus has been reached about frontal stents use. Here we introduce the experience of using a new omega shaped silicon stent, which has shown promising results in keeping the frontal sinus opening patent.
IntroductionFrontal sinus surgery is challenging due to its anatomical complexity and difficulty of access. The small size, proximity to the orbit and skull base, along with its anterior position and orientation, all play a role as contributing factors [1]. Revision frontal sinus surgery is even more challenging. Numerous studies have documented outcomes using various techniques, yet maintaining long-term sinusotomy patency remains a significant challenge.
To reduce the occurrence of synechiae and stenosis, stents have been developed. Their main purpose is to keep wound edges apart, preventing the formation of synechial bands and subsequent narrowing [2,3]. Additionally, they occupy space that might otherwise fill with blood, fibrin, or mucus, thereby lessening the need for post-operative cleaning [2]. Stents also serve as a framework to support epithelial growth, particularly in regions where the bone surface is exposed [2]. Frontal sinus stents have been used with an objective of improving the outcome since the early 1900s using numerous materials and techniques, no definite consensus however [4,5]. This paper describes our experience of using omega shaped frontal sinus stent made out of silicon rubber drain in case of Draf IIb procedure.
MethodsPatientsPatients who underwent the Draf IIb procedure between January 2019 and September 2024 were identified and included in the study using medical records from Chungnam National University Hospital. This study was approved by IRB No. 2024-12-009. Patients with a follow-up period of less than 3 months after surgery were excluded from the study. Surgery was carried out in cases such when sinusitis would not be handled with medication or benign tumor such as inverted papilloma that required opening of frontal sinus existed. Patients went through thorough medical history taking, nasal endoscopy, and ostiomeatal unit or paranasal sinus (PNS) CT to evaluate the sinus structures and disease extent beforehand. If adequate width is not acquired, that is a minimum of 1 cm on A-P diameter, or exposure of bone and mucosal injury are too much, stent insertion is considered.
Technical descriptionThe choice to perform the Draf IIb procedure was largely guided by intraoperative observations. This approach was favored when the Draf IIa opening appeared inadequate and likely to develop post-operative stenosis or when greater access was required, such as for treating tumors or mucoceles.
In performing the Draf IIb frontal sinusotomy, the anterior portion of the middle turbinate, including the part attached to the frontal sinus floor, was removed using through-cutting forceps up to the level of the cribriform plate. Next, the frontal sinusotomy was extended to the nasal septum by removing the frontal sinus floor and enlarged anteriorly by removing the frontal beak using a 70° diamond drill. Again, if the A-P diameter is less than 1 cm or if there is significant bone exposure and mucosal damage, the use of a stent is considered.
A silicon drain (Med Vac 100 mL 3.2 OD, 1.6 ID; Hyupsung Medical Co., Ltd) is made to a shape of an omega (Fig. 1). The bottom of the omega head is sutured with 4-0 nylon 2-3 times, about 3 mm apart between each stitch to form a short neck. The head of the stent is automatically spread inside the frontal sinus after insertion which gives an anchoring effect, thus making suturing unnecessary. This effect also helped the stent from dislodging due to nasal irrigation or nose blowing. For a mean frontal sinus dimensions at 16 years were 12.8±5.0 mm (antero-posterior)/21.9±8.4 mm (cranio-caudal)/24.5±13.3 mm (transverse) according to Barghouth, et al. [6], the size of omega head is formed to be approximately 2-3 cm. The omega head takes up an adequate amount of space that it not only helps secretion to be drained but also prevents stenosis to occur. The legs of the omega are cut to the size that at least one of them can be placed in the other sinus cavity, which is already opened from the surgery (Fig. 2A).
Post-operative carePost-operative PNS x-ray at the day of the surgery is taken to confirm whether the stent is placed in the right place (Fig. 2B). The patient is discharged a day after the surgery, and is instructed to use nasal irrigation at least 3 times a day and apply topical nasal steroids twice a day. During the routine follow up, nasal debridement is done if too much nasal crust or discharge accumulates that it hinders the function of the stent (Fig. 2C). The stent is removed after at least 9 months the insertion at an outpatient visit (Fig. 2D). Fig. 2E shows the endoscopic pictures of the patients months after removal of the stent. Removal is easily carried out even only with topical anesthesia, without definite damage to the nasal mucosa as well. Patients are instructed to visit regularly with 3 to 6 months intervals for observation.
ResultsOut of 3311 patients who received endoscopic frontal sinus surgery from 2019 January to 2024 September, total of 25 patients were underwent Draf IIb procedure, and 16 patients (16 sides) were inserted of a frontal stent (Table 1). The diagnosis of the 16 patients was chronic rhinosinusitis with nasal polyposis in 6 patients, frontal sinusitis in 6 patients, inverted papilloma in 3 patients, and mucopyocele in 1 patient. Nine patients had prior surgery and were revision cases. The frontal stent was maintained for a period ranging from 9 to 60 months before being removed. Out of 11 sides of which we removed the stent, patency was maintained in the 10 sides at the latest follow up.
One of the patients whose stent was removed, we had a trouble of getting it out because the stent neck was tightly stuck that the patient complained of pain thus he had to go under general anesthesia to get rid of it. During the healing process, the knot seemed to be entangled with injured mucosa. We are keeping our surveillance over remained 5 patients until the right time for a removal is reached.
DiscussionTaking in count the complexity regarding the frontal sinus surgery, many surgery techniques have been introduced, Lynch procedure, Draf type II, and extended modified Lothrop procedure. These approaches allow widened common outflow tract from frontal sinus to be created, but also increasing patient morbidity and face inherent complications [7]. Repeated operation of frontal sinus is definitely unfavorable in that manner.
Frontal sinus opening stenosis can occur due to causes such as post-operative scarring and neo-osteogenesis [8]. We believe frontal stents can some extent prevent those processes, and therefore introduce the experience of using new omega shaped silicon stent.
Previous study reported that frontal sinus stenting is indicated in cases where the opening diameter is less than 5 mm, where there is purulence, osteitic bone, granulomatous inflammation due to vasculitis, stenosis from prior failed sinus surgery, lateralization of the middle turbinate, exposed bone in the frontal recess, severe polyposis, or the patient has aspirin intolerance [3]. All of our cases were patients who underwent Draf IIb, so there was a lot of denuded bone, and some patients needed a stent because the opening diameter was narrow.
There have been reports on complications after frontal sinus stent insertion that were introduced previously [9]. We believe the omega silicon stent has some advantages over other frontal sinus stents that it more likely can avoid complications and the related technique is simpler to implement. First, the omega silicon stent’s head design automatically locks the stent in its place that no suturing is needed that migration is unlikely to occur. The head design also makes easier for the operator to grasp the head with forceps, place the stent at the entrance of the frontal sinus opening. The stent can be easily pushed inside the sinus by pushing the neck, or the “crotch” between two stent legs. The material of the stent, which is silicon drain and a nylon 4-0 are easily accessible, typical surgery tools that surgeons use, that anyone who can suture can simply make at the spot. Surgeon can choose a drain size according to the size of the frontal sinus opening that he made, which decreases the possibility of pain caused by the stent giving much pressure to the frontal sinus or the opening. Although very low in possibility, secondary infection, hypersensitivity, bacterial biofilm, toxic shock syndrome and granulomatous tissue formation have been mentioned as stent complications in previous papers [9]. During our follow up period of the patients, the aforementioned complications were not observed. However, the number of patients included in this study is limited that longer follow up period is needed to confirm.
Whether frontal sinus stenting truly result in favorable surgery prognosis is still a subject of debate, for a limited number of studies elaborate on their success [9]. Also, no consensus exist about indwelling period of the stent that it varies according to surgeon by surgeon. Freeman and Blom [10] kept stents in situ for six to 12 months when treating re-stenosis, but only for four weeks to prevent stenosis after a primary surgical procedure. One study found that frontal sinus stents left in situ for more than six months were more effective than stents removed earlier [11].
Adequate post-operative care is necessary all the more after stent insertion to maintain the stent’s purpose. Careful regular debridement in the outpatient department with perpetual nasal irrigation with use of topical steroid spray at patient’s home should be executed.
It has not been long since we adopted this omega shaped frontal stent insertion, and thus the number of patients lack to reflect the valid effectiveness of the stent. Nonetheless, what we have experienced may pave the way for this new shaped silicon stent for we have seen a promising outcome.
Supplementary VideoThe Supplement is available with this article at https://doi.org/10.3342/kjorl-hns.2024.00584.
Fig. 2.Postoperative status of patients. A: The omega shaped stent inserted into frontal sinus. B: Post-operative PNS x-ray which shows the omega stent is well inserted into the frontal sinus. C: Outpatient endoscopy after surgery showing the stent inserted into the frontal sinus. D: Outpatient endoscopy right after removal of the stent showing patent frontal sinus opening. E: Outpatient endoscopy months after removal of the stent showing frontal sinus opening remains patent (1st picture: 3 years postop, 3 months after stent removal. 2nd picture: 1.5 year postop, 1 year after stent removal). 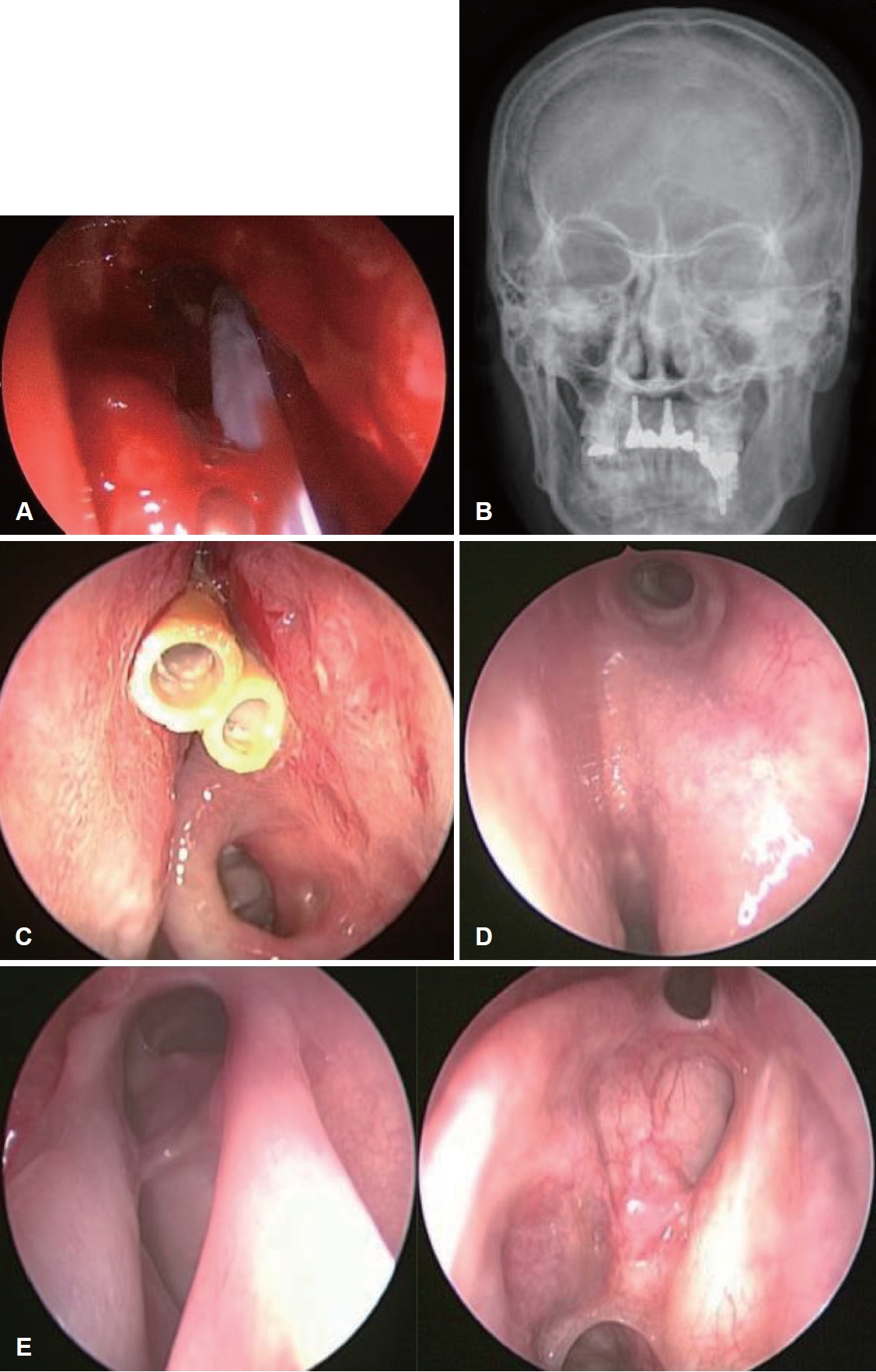
Table 1.Our experiences of frontal stenting in Draf IIb procedure REFERENCES1. Banhiran W, Sargi Z, Collins W, Kaza S, Casiano R. Long-term effect of stenting after an endoscopic modified Lothrop procedure. Am J Rhinol 2006;20(6):595-9.
2. Mansour HA. Double J stent of frontal sinus outf low tract in revision frontal sinus surgery. J Laryngol Otol 2013;127(1):43-7.
3. Reeve NH, Ching HH, Kim Y, Schroeder WW. Possible skull base erosion after prolonged frontal sinus stenting. Ear Nose Throat J 2021;100(5):NP218-21.
4. Bandino F, Bates J, Qureishi A, Martinez-Devesa P. The use of modified Montgomery T-tubes as frontal sinus stents: how I do it. J Laryngol Otol 2022;136(12):1328-9.
5. Bandino F, Pendolino A, Bates J, Qureishi A, Martinez-Devesa P. Frontal sinus stenting in endoscopic sinus surgery: the 10-year Oxford experience. J Laryngol Otol 2024;138(1):60-6.
6. Barghouth G, Prior JO, Lepori D, Duvoisin B, Schnyder P, Gudinchet F. Paranasal sinuses in children: size evaluation of maxillary, sphenoid, and frontal sinuses by magnetic resonance imaging and proposal of volume index percentile curves. Eur Radiol 2002;12(6):1451-8.
7. Hunter B, Silva S, Youngs R, Saeed A, Varadarajan V. Long-term stenting for chronic frontal sinus disease: case series and literature review. J Laryngol Otol 2010;124(11):1216-22.
8. Gross CW, Schlosser RJ. The modified Lothrop procedure: lessons learned. Laryngoscope 2001;111(7):1302-5.
|
|
||||||||||||||||||||||||||||||||||||||||||||||

 |
 |